The incidence and prevalence of diabetes, also known as diabetes mellitus (DM), are increasing globally, especially in industrialized countries in recent years. Approximately 30-70% of diabetes patients experience skin manifestations during the chronic progression of the disease.
1. Skin Manifestations Related to Diabetes
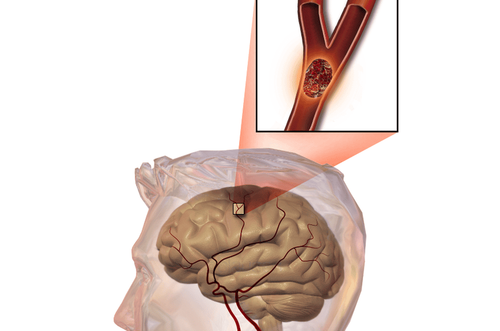
Imbalanced insulin hormones and elevated blood sugar levels in diabetic patients lead to metabolic, vascular, neurological, and immune abnormalities. Organs that can be damaged by diabetes include the cardiovascular system, kidneys, nervous system, eyes, and skin. Many patients are only definitively diagnosed with diabetes when these internal organs are damaged. Recognizing the risks of carbohydrate metabolism abnormalities can help diagnose diabetes early and prevent complications. Skin manifestations can help detect diabetes, while diabetes can also exacerbate skin diseases. Approximately 30-70% of diabetes patients exhibit skin manifestations during the chronic progression of the disease.
Below are some skin manifestations related to diabetes:
- Diabetic Foot: Diabetic foot is characterized by ulcers on the foot due to diabetes combined with peripheral neuropathy (60-70%) and ischemia caused by peripheral vascular inflammation leading to poor blood circulation (15-20%) or both causes. Ulcers may occur in pressure areas on the foot, potentially causing complications like infection and gangrene.
- Diabetic Dermopathy: Diabetic dermopathy presents as reddish-brown skin patches. This is a small vessel disease and is the most common skin sign of diabetes, occurring in more than 50% of diabetic patients, and is twice as common in men as in women. Lesions often appear on the shins, and sometimes on the thighs and arms. Diabetic vascular complications can occur in patients with dermopathy-related small vessel lesions, such as retinopathy, neuropathy, and nephropathy.

- Necrobiosis Lipoidica: Necrobiosis lipoidica occurs in about 1% of diabetic patients, with over 70% being women. The cause is unknown but may be due to inflammation of small blood vessels in diabetes. Insulin-dependent diabetes patients may develop necrobiosis lipoidica early, averaging around age 22, while it appears later in non-insulin-dependent diabetes patients or non-diabetic individuals, averaging around age 49.
- Acquired Ichthyosiform Changes of the Shin: Itching of the shins is a common skin manifestation in diabetic patients, particularly in 50% of young insulin-dependent diabetes patients, with an unknown cause. It may be due to small vessel disease, cornified layer adhesion, increased glycosylation, and accelerated skin aging.
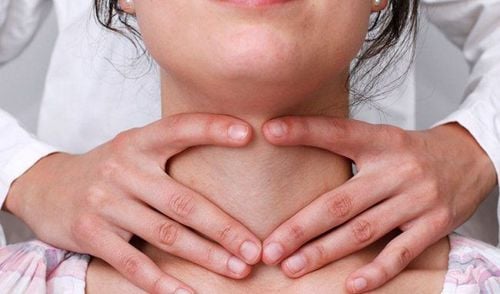
- Acanthosis Nigricans: This presents as smooth, velvety, thickened, and hyperpigmented skin on folds such as the neck, armpits, groin, navel, areola, under the breasts, and elbows. This is common, especially in insulin-resistant type A diabetes patients, often accompanied by obesity, a component of metabolic syndrome. The cause is elevated insulin levels, which can activate insulin growth factor (IGF-1) receptors on keratinocytes, leading to epidermal growth. Malignant forms are rare.
- Skin Tags (Acrochordons): These are benign skin growths with a stalk. They commonly occur around the neck or large body folds in elderly individuals. Some diabetes patients develop skin tags along with acanthosis nigricans. Researchers suggest that people with numerous skin tags are at a higher risk of diabetes due to carbohydrate metabolism disorders.
- Eruptive Xanthomas: Eruptive xanthomas are small, reddish-yellow papules, 1-4 mm in size. Lesions occur in outbreaks and can coalesce into larger patches. Experts suggest that eruptive xanthomas may be an early indicator of untreated diabetes with severe hypertriglyceridemia.
- Scleroderma-like Skin Changes: This condition presents as thickened and hardened skin on the back of the fingers (sclerodactyly) and the proximal or middle interphalangeal joints. Symptoms may affect the forearms, upper arms, and back, symmetrically and without pain. The skin feels waxy, without atrophy, telangiectasia, swelling, or Raynaud's phenomenon.
This occurs in 10-50% of diabetes patients, equally in men and women, predominantly in type I diabetes. The cause is advanced glycosylation end products thickening collagen. - Scleredema Diabeticorum of Buschke: This presents as diffuse, symmetrical skin thickening, sometimes with erythema, mainly on the neck, shoulders, back, and occasionally the face. The skin becomes woody, non-pinchable, and less sensitive to pain. This is rare, primarily occurring in men over 40 with type II diabetes and rarely in women. Most patients develop multiple complications, start insulin dependence, and treatment is often unsuccessful.
- Bullosis Diabeticorum: These are tense blisters, 0.5-3 cm in size, without inflammatory rings, usually appearing on the fingers, hands, forearms, toes, feet, and legs, rarely on the trunk. These rare lesions develop acutely, often without itching or pain, and occur in severe diabetes patients. One early sign of diabetes is the appearance of blisters on the lower extremities.

- Kyrle Disease (Acquired Perforating Dermatoses - APD): APD lesions are chronic inflammatory granulomas around hair follicles, resembling oyster shells, with hyperkeratotic centers, extremely itchy, forming long streaks (Koebner phenomenon), red or pink in white patients, and hyperpigmented in black patients, appearing on the trunk, extremities, scalp, and face. Researchers have not yet determined the exact cause of APD, which may be a secondary inflammatory response to uremia, uric acid deposits, or scratch-induced trauma. APD is closely associated with 5-10% of diabetes patients and chronic kidney disease, typically appearing 10-30 years after diabetes diagnosis and several months after dialysis.
- Rubeosis: This condition occurs in about 3%-59% of diabetes patients, presenting as persistent facial, neck, and extremity redness, possibly due to decreased vasoconstriction.
- Carotenoderma: Orange-yellow skin color occurs in areas with active sebaceous glands (face) and thick stratum corneum (hands, feet), possibly affecting nails.
- Keratosis Pilaris: This common benign skin condition presents as hyperkeratotic papules around hair follicles, primarily on the trunk. During diabetes progression, keratosis pilaris, resembling acquired ichthyosis, appears early.
- Eruptive Xanthomas: Symptoms include sudden outbreaks of yellow or reddish-brown papules across the body, mainly on the backs of hands, feet, shins, and trunk, commonly in young men with type I diabetes. Lesions consist of dermal macrophages loaded with triglycerides, differing from cholesterol ester xanthomas. These occur in diabetes patients with elevated triglycerides.
- Skin Infections (Fungal and Bacterial): Skin infections affect 20-50% of diabetes patients, predominantly type II diabetes with poor blood glucose control, leading to microcirculatory
Fungal infections:
In diabetic skin infections, fungi account for the highest proportion because the patient has a weakened skin barrier, the most common is Candida infection and this is often the first warning sign of diabetes. Intertrigo, stomatitis, nail inflammation, balanitis, vulvovaginitis can also be caused by Candida infection.
Other fungal skin infections of diabetes are often: athlete's foot, erysipelas, cellulitis, more serious is fungal sepsis. Diabetic ketoacidosis patients are at high risk of infection with Phycomycetes fungi (mucormycosis) causing central vascular necrosis, especially in the pharynx, can cause encephalitis and most patients die.
Bacterial Infections:
Compared to other diseases, bacterial skin infections in diabetic patients are three times more common, mostly due to Gram-negative bacteria like Pseudomonas aeruginosa. This is especially concerning in diabetic foot ulcers, which should not be taken lightly because they can lead to limb amputation, severe sepsis, and drug-resistant P. aeruginosa. Diabetic patients are also highly susceptible to pyoderma, erysipelas, and cellulitis caused by Group A & B Streptococcus, and methicillin-resistant Staphylococcus aureus (MRSA) if blood sugar is not well controlled.

2. Skin Complications from Diabetes Treatment
Using antidiabetic medications can cause some skin reactions, such as urticaria, erythema multiforme, acneiform rashes, and lichenoid drug eruptions. Photosensitivity reactions can occur due to drugs like Tolbutamide and Chlorpropamide. Sulfonylureas are the class of hypoglycemic drugs most likely to cause allergic skin reactions. Compared to the first generation, second-generation Sulfonylureas cause fewer side effects.
Lipodystrophy at insulin injection sites, usually the abdomen and thighs, can occur 6-24 months after starting injections, more common in children and women. Lipohypertrophy: This occurs in 20-30% of patients with type I diabetes and 4% with type II diabetes, particularly at sites of frequent, high-dose insulin injections with repeated use of needles without rotating sites. These are soft, fatty-like lumps in the skin. Injecting insulin into these lipohypertrophy sites can delay insulin absorption, leading to erratic blood sugar control and unpredictable hypoglycemia episodes. Allergic reactions to insulin are rare. Human insulin, produced using recombinant DNA technology, causes fewer allergic reactions and lipodystrophy.
Allergic skin reactions to insulin can include urticaria or delayed hypersensitivity reactions (serum sickness).

3. Causes of Itchy Hands and Feet
When your hands and feet itch, appropriate treatment can help alleviate the symptoms. However, how you treat the itch depends largely on the underlying cause, including:
- Dry skin: Could be due to winter weather or over-scrubbing.
- Psoriasis: Itchy hands and feet could signal an underlying health condition like psoriasis.
- Eczema: This term refers to a group of conditions that cause skin inflammation.
- Scabies: A type of eight-legged mite, known as the human itch mite, causes this common skin condition. These tiny insects burrow into the top layer of the skin and lay eggs, causing scabies.

Diabetes can also cause itchy hands and feet:
- Some skin issues can be the first signs of diabetes. For example, Xanthomatosis, a condition caused by uncontrolled diabetes, can make your hands and feet itch. This symptom disappears once diabetes is well managed.
- Xanthomatosis can also cause itching on the arms, legs, and buttocks and lead to other issues like small skin bumps and high cholesterol levels. Allergies: Your skin may react allergically to substances you have touched, known as allergic contact dermatitis.
4. Reducing the Impact of Itchiness from Diabetes
Itch treatment is most effective when the exact cause is identified.
Additionally, to limit the impact of itchiness, diabetic patients should follow a reasonable diet and lifestyle:
Consume foods rich in fiber, low in cholesterol, and low in saturated fats. Limit refined grains and instead opt for whole grains, and include various forms of protein in each meal.

Maintain a relaxed mind: Avoid letting worries and stress about illness affect your life.
Worrying not only fails to improve your condition but can even exacerbate it. Exercise regularly: Physical activity can help control blood sugar levels. Moreover, regular exercise helps your body use insulin more effectively.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.
Reference source: webmd.com