This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Eosinophilic esophagitis (EoE) is an immune-mediated clinical condition presenting with symptoms of esophageal dysfunction and esophageal eosinophilia. Because of the presence of eosinophilia and response to PPI therapy, GERD and PPI-REE have become the most common alternative diagnoses for EoE.
Abbreviated terms:
EoE: Eosinophilic esophagitis: esinophilic esophagitis
GERD: Gastroesophageal reflux disease: Reflux esophagitis
IL: Interleukin: Interleukin factor
PPI: Proton pump inhibitor: Proton pump inhibitor Proton pump
PPI-REE: Proton pump inhibitor-responsive esophagal: Proton pump inhibitor-responsive esophagitis
Eosinophilia: eosinophils
VTQBCAT: eosinophilic esophagitis
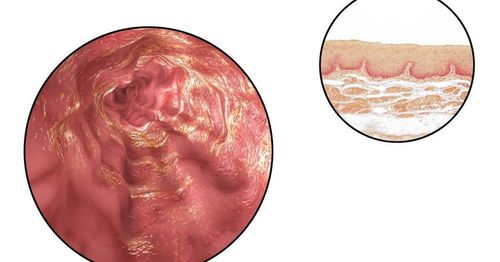
1.What is eosinophilic esophagitis? Eosinophilic esophagitis (EoE) is an immune-mediated clinical condition presenting with symptoms of esophageal dysfunction and esophageal eosinophilia with 15 eosinophils. acidosis on an optical field when viewed under a microscope in the absence of other known causes. Eosinophilic infiltration into the esophagus is not unique to EoE, but is present in gastroesophageal reflux disease (GERD) and several other conditions including inhibitory esophageal eosinophilia. proton pump (PPI-REE). Because of the presence of eosinophilia and response to PPI therapy, GERD and PPI-REE have become the most common alternative diagnoses for EoE.
PPI-REE is a condition in which a patient has clinical and histological findings suggestive of EoE, but complete remission of symptoms and esophageal eosinophilia on PPI therapy. PPI-REE was first described in 2006 when three patients with esophageal eosinophilia, dysphagia, swallowing and vomiting reported histological and symptomatic responses to treatment. PPI lasts 8 weeks. At the time, the authors questioned whether this clinical response might be due to allergic eosinophilic esophagitis or to gastroduodenal esophagitis. Since then, PPI-REE has been recognized as a separate clinical entity, with subsequent studies demonstrating a histological response to PPIs in 33-74% of patients with symptoms of true eosinophilia. manage. Therefore, both the 2011 and 2013 EoE guidelines state that PPI-REE should be excluded in all patients with esophageal eosinophilia by treatment with an 8-week course of any PPI, usually 20–40 mg twice daily, followed by endoscopy to assess histological response.
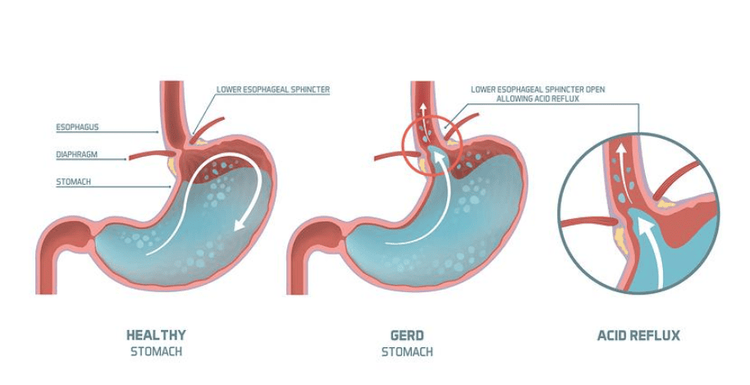
The well-documented overlap between PPI-REE, GERD, and EoE leads to challenges in differentiating these conditions. GERD can cause esophageal eosinophilia that is responsive to PPI therapy, similar to PPI-REE. In addition to acid-peptide injury, cytokine-mediated pathways have been suggested to induce esophagitis in GERD, and some of these pathways may overlap with EoE. Therefore, it remains an unanswered question whether PPI-REE is a subtype of GERD, a subtype of EoE, or a different clinical entity altogether. The aim of this paper is to discuss the clinical, endoscopic and histological features, pathogenesis and pathogenesis of PPI-REE, and to highlight the similarities and differences with EoE.
2. Clinical presentation of PPI-REE 2.1. Symptoms and clinical features The clinical presentation of EoE varies in adults and children, but many studies have shown that it is almost identical to that of PPI-REE. Children with EoE often have upper gastrointestinal symptoms such as abdominal pain, nausea, vomiting, food intolerance, and poor growth. In adults, common symptoms are swallowing solid foods, food reaction disturbances, heartburn, and noncardiac chest pain. Not only are the symptoms presenting the same in PPI-REEs, but there is also a strong association with allergic diseases such as asthma and allergies in both conditions.
Like EoE, PPI-REE tends to occur mainly in Caucasian males. While some studies have suggested that adult patients with PPI-REE may be slightly older than EoE patients, a recent meta-analysis of 10 studies found that the two conditions clinically indistinguishable.
2.2. Endoscopic findings Esophageal ring, linear groove, white plaque, and exudate, although not diagnostic, are characteristic endoscopic findings of EoE. The esophagus can also narrow and develop into an obstruction due to chronic fibrosis. In a large prospective study, PPI-REE patients had similar endoscopic findings, but were less likely to have annulus, stenosis, stenosis, and hypovascularity compared with EoE patients. However, these differences were not statistically significant in multivariate analysis and cannot be used to distinguish EoE from PPI-REE. Another study by Moawad et al. also showed no difference in endoscopic findings between PPI-REE and EoE.
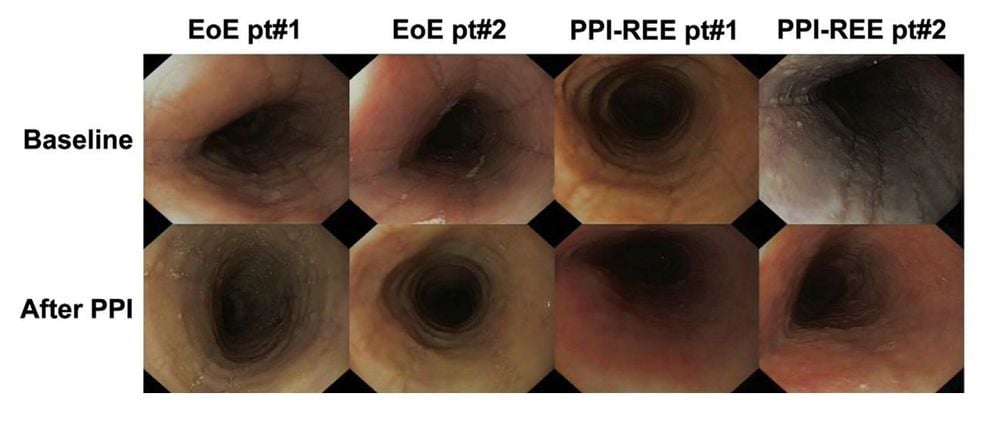
2.3. Histological findings Histologically, EoE is characterized by esophageal eosinophil infiltration with ≥15 eosinophils on high-powered media. Additional findings include eosinophilia, eosinophil microabsorption, basal layer hyperplasia, elongation of rete-pins, dilated intracellular spaces (also called spongiform disease). ) and stromal fibrosis. As with endoscopic and clinical features, there were no differences in baseline eosinophil counts or other relevant histopathological features to distinguish PPI-REE (before PPI administration) from EoE.
In summary, both retrospective and prospective studies in adults and children with esophageal eosinophilia did not reveal significant differences in the clinical, endoscopic and histological manifestations of PPI-REE and EoE. While small differences in individual characteristics have been noted in several studies, after multivariate analysis, no one was able to distinguish EoE from PPI-REE independently. This lack of clinical distinction has prompted investigations into alternative diagnostic modalities.
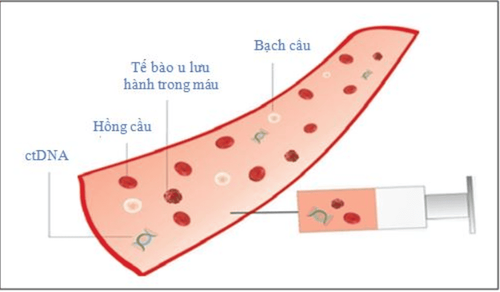
3. Role of GERD and the role of esophageal pH testing as a diagnostic tool for PPI-REE Due to the difficulties in distinguishing PPI-REE from EoE on clinical, endoscopic, and histological grounds , a reasonable question is whether pH monitoring is useful. The presence of intraepithelial eosinophils in esophageal biopsies was proposed as a diagnostic criterion for reflux esophagitis more than 30 years ago, and since then it has been appreciated that GERD may be associated with esophagitis. associated with high levels of esophageal eosinophils. Therefore, one can hypothesize that GERD underlies PPI-REE. There may be a complex relationship between reflux, EoE, and esophageal eosinophilia, and the initial guidelines for EoE consider PPI response as a marker of GERD. While individual patients with PPI-REE may have some features suggestive of GERD (eg, large hernia, erosive esophagitis, symptoms mainly heartburn, older age, absence of symptoms). currently allergic, responsive to PPIs), the majority of patients reported with PPI-REE have more EoE clinical phenotype than GERD imaging.
Several studies examining pH testing in PPI-REE demonstrate that the presence or absence of pathological esophageal acid exposure does not reliably predict PPI response. In a prospective study by Francis et al of 51 subjects with >15 eosinophils per field, those with abnormal pH studies were treated with high-dose PPI therapy (twice a day). , while those with normal pH studies were treated with topical steroids. About two-thirds of patients have normal esophageal pH monitoring tests, suggesting that acid reflux is likely not the cause of esophageal eosinophilia. Among those with abnormal acid reflux, nearly 40% did not respond histologically to PPI treatment. Similar results were seen in a retrospective cohort study by Dranove et al., in which 59% of patients with a positive esophageal pH-monitoring study did not respond histologically to PPI therapy. Therefore, abnormal acid exposure is not the cause of many cases of PPI-REE, and a positive pH test does not accurately predict the response of esophageal eosinophilia to PPIs.
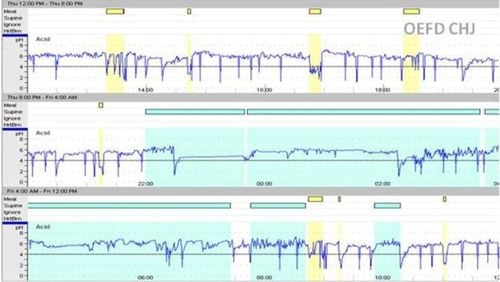
A normal esophageal pH test is also a poor predictor of PPI response in patients with esophageal eosinophilia. In several studies of patients who had esophageal biopsies with 15 eosinophils per field and no pathological acid reflux by esophageal pH monitoring, 18–45% responded to therapy. PPI. This PPI response to a normal pH study argues against GERD or acid-based etiology in many cases. Therefore, the available data do not support pH testing as a useful predictor of PPI response for patients with esophageal eosinophilia.
PPI-REE was only recently recognized and knowledge about the condition is rapidly growing. Initially, PPI-REE was thought to have a very close relationship, namely a manifestation of GERD. In this initial framework, GERD and EoE were considered separate conditions, and PPI-REE may overlap with GERD but not with EoE. However, the interplay between GERD, EoE, PPI-REE and esophageal eosinophilia is now known to be complex with significant overlap and can be re-conceptualized in a number of ways. Emerging data suggest that PPI-REE shares many similarities with EoE and is in fact indistinguishable from EoE in its clinical, endoscopic, and histological manifestations. Mechanistically, tissue expression of inflammatory markers such as MBP, eotaxin-3 and tryptase was the same as in EoE. Both conditions share a very similar genetic expression profile, but it is likely that selected genes differentially expressed in PPI-REE and EoE could predict PPI response. While there is ample evidence that PPI-REE may be a subtype of EoE, further elucidation of the natural history of the disease, immune-mediated basis, and optimal dosing of PPI regimens is required. and long-term effects of PPI use. More importantly, the description of PPI-REE as a subtype of EoE may have clinical implications in terms of disease management, possibly in relation to PPI as a first-line treatment for all EoE patients and only switch to steroids and dietary therapy in nonresponders. Although the data still do not fully support such an apparent paradigm shift, the rapid evolution of EoE definitions and the change in understanding of PPI-REE imply that revision of the diagnostic and management algorithms are likely to occur in the future, the rapid evolution of EoE definitions and the change in understanding of PPI-REE imply that modifications to the diagnostic algorithms and management is likely to occur in the future the rapid evolution of EoE definitions and the change in understanding of PPI-REE imply that modifications to the diagnostic and management algorithms may be will happen in the future.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Swathi Eluri, MD 1, 2 and Evan S. Dellon, MD MPH. PPI-responsive esophageal eosinophilia and eosinophilic esophagitis: More similarities than differences. Curr Opin Gastroenterol. 2015 July; 31 (4): 309–315. Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. The Journal of allergy and clinical immunology. 2011;128(1):3–20. e6. quiz 1–2. Epub 2011/04/12. [PubMed] [Google Scholar] 2. Dellon ES, Gonsalves N, Hirano I, Furuta GT, Liacouras CA, Katzka DA. ACG clinical guideline: Evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE) The American journal of gastroenterology. 2013;108(5):679–692. quiz 93. Epub 2013/04/10. [PubMed] [Google Scholar]