This is an automatically translated article.
The article is professionally consulted by Master. BSCK II Phan Thi Minh Huong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Da Nang International General Hospital.Cholestasis is a condition in which the bile outlet is blocked inside or outside the liver, allowing bile to enter the bloodstream, causing jaundice. If the root cause of obstructive jaundice is a malignancy, the best and long-term outcome for the patient is surgical removal of the tumor.
1. What is obstructive jaundice?
Jaundice is a yellow tinting of the skin and mucous membranes of the eyes caused by an increase in bilirubin beyond normal limits in the blood.Normal total bilirubin in the blood is 0.8-1.2mg/dl, in which indirect bilirubin is 0.6-0.8 mg/dl and direct bilirubin is 0.2-0.4 mg/dl
Jaundice is evident when bilirubin TP > 2.5 mg/dl
Subclinical jaundice when bilirubin TP: 2- 2.5 mg/dl
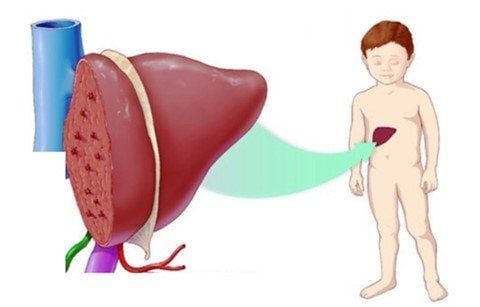
Obstructive jaundice is a yellowing of the skin with direct hyperbilirubinemia due to biliary obstruction, blocked bile ducts can be intrahepatic or extrinsic liver.

Vàng da tắc mật là tình trạng vàng da tăng bilirubin trực tiếp do bế tắc đường mật
2.Diagnosis of obstructive jaundice
2.1 Differential diagnosis First of all, it is necessary to distinguish between the two types of intrahepatic and extrahepatic cholestasis.Clinically: there is a large gallbladder, prolonged discolored stools, definitely extrahepatic cholestasis. Intrahepatic cholestasis never had that symptom. Ultrasound: Is the most important method today to distinguish two types of cholestatic jaundice. 95% gives accurate results, cholestasis in the liver does not dilate the biliary tree. Extrahepatic cholestasis results in dilated bile ducts and enlarged gallbladder. Computerized tomography of the liver with drugs to determine the cause Cholangiography injects contrast directly into the bile ducts
Intrahepatic cholestasis: bile ducts remain clear Extrahepatic cholestasis: large bile ducts are obstructed and dilated Feces Differentiation of jaundice from different causes : Hemolytic jaundice: increased indirect bilirubin in the blood, jaundice accompanied by anemia never with itching or discolored stools And hematologic tests showing hemolysis: strength decreased erythrocyte stability, coombs test, increased reticulocyte count, increased serum iron... Jaundice due to congenital diseases (Gilbert and Dubin Johnson's disease), only indirect bilirubin or TT was seen in the blood increased, other than that no any other clinical and laboratory changes. Patients can still live long. This disease is rare. 2.2 Diagnosis of the cause To diagnose the cause of cholestasis should be based on:
Clinical symptoms: Each cause has its own clinical picture. Cholangiography: with many methods: oral contrast, contrast injection, endoscopic retrograde scan, direct needle puncture into the biliary tree. These methods can very well diagnose the cause of extrahepatic cholestasis. Ultrasound: can also diagnose the cause. For example, look for choledocholithiasis, gallstones, bile duct thickening and narrowing in cholangiocarcinoma, hyperechoic mass in liver K. Liver biopsy: very valuable to diagnose the cause of intrahepatic cholestasis but for extrahepatic cholestasis is contraindicated. Other special tests depend on the cause. Examples: A.F.P for liver K, angiography for pancreatic head or liver tumor, immunoassay for primary biliary cirrhosis.
3. Treatment of obstructive jaundice
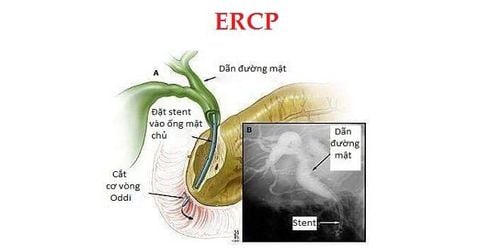
Bác sĩ có thể khuyên người bệnh nên làm thủ thuật ERCP để điều trị vàng da tắc mật
Your doctor may recommend an ERCP procedure, a percutaneous transhepatic cholangiogram (PTC) with percutaneous bile drainage. Essentially, this allows the drainage of bile that has been stagnant in the liver out.
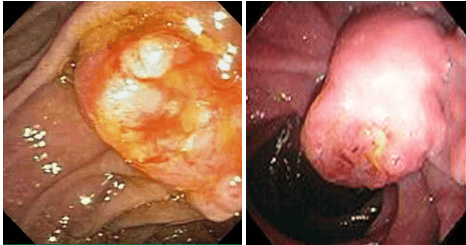
Definitive treatment depends on the cause of the jaundice. If gallstones are diagnosed, endoscopic removal of stones obstructing the bile duct is recommended. Endoscopic stenting is sometimes necessary, as a temporary measure to relieve the common bile duct obstruction and clear the infection before definitive surgery.
Then, laparoscopic cholecystectomy is indicated to remove the gallbladder, which contains many gallstones.
If the root cause of obstructive jaundice is a malignancy, the best and long-term outcome for the patient is surgical removal of the tumor.
Most patients have melanoma and surgery is often not suitable, so chemotherapy or radiation therapy would be the next best option.
For these patients, obstructive jaundice may be relieved through stenting with endoscopic or radiological guidance, once the diagnosis of cancer is confirmed.
Doctor Huong has over 30 years of experience in the field of Gastroenterology in which with nearly 20 years holding the position of Deputy Department, Head of Department of Hue Central Hospital. Currently, he is a Doctor of Gastroenterology - Gastrointestinal Endoscopy - General Internal Medicine Department of Vinmec Da Nang International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.