This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Eosinophilic esophagitis (eosinophilic esophagitis) is a chronic, immune-mediated disease caused by food allergens, presenting with symptoms of dysfunction oesophagitis and esophagitis predominated by eosinophils.
1. When to suspect and how to diagnose eosinophilic esophagitis?
Eosinophilic esophagitis affects children and adults of all ages of all races and ethnicities, with reports of eosinophilic esophagitis from countries around the world . Eosinophilic esophagitis affects both sexes but men predominate by a factor of about 3 to 1. Physicians should suspect eosinophilic esophagitis when patients present with symptoms of dysfunction. esophageal capacity.
Esophageal dysphagia is reported by 60-100% of patients with eosinophilic esophagitis and more than 25% of these patients have experienced regurgitation. Patients often complain of chest pain, heartburn, and upper abdominal pain.
2. What should be taken from the patient's history if eosinophilic esophagitis is suspected?
A history of allergic disease such as rhinitis, asthma, or atopic dermatitis is found in 50-60% of patients with eosinophilic esophagitis. In addition, a family history of eosinophilic esophagitis or dysphagia will further increase your clinical suspicion for eosinophilic esophagitis.
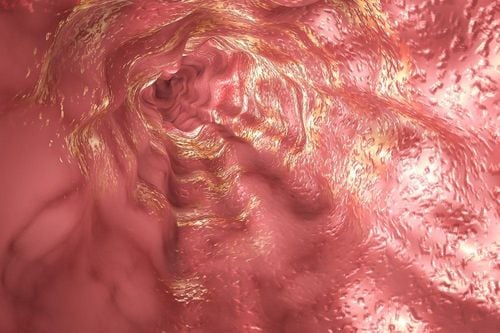
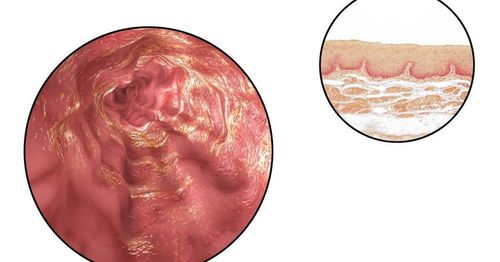
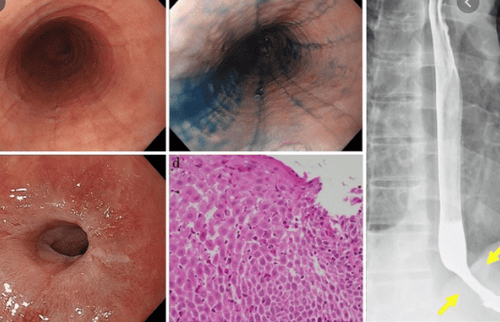
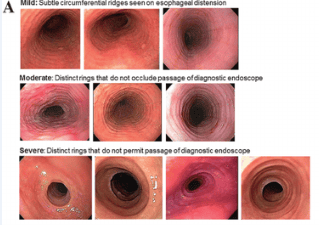
2.1 Signs on Endoscopy When endoscopy is performed, endoscopic signs of eosinophilic esophagitis are evaluated. The endoscopic features of eosinophilic esophagitis were described using the endoscopic eosinophilic esophagitis reference point, EREFS, which stands for features with exudative, mucosal ring. conjunctiva, edema, and longitudinal grooves were detected on endoscopy.
However, there are no features specific for eosinophilic esophagitis and the esophagus may appear completely normal in about 5-10% of cases. Esophageal biopsy showing at least 15 eosinophils on a high-magnification field (microscope field) is required for diagnosis. Other typical histological findings include eosinophilic microabsorption, basal and/or papillary hyperplasia, and dilated intercellular spaces. There may also be prominent fibrosis in the stroma.
Therefore, a patient with symptoms of esophageal dysfunction and at least 15 eosinophils on a high-magnification field on an esophageal biopsy would be suspected of having eosinophilic esophagitis. eosinophil esophagitis, but eosinophilic esophagitis was diagnosed only after other non-eosinophilic esophagitis disorders (i.e. vasculitis, eosinophilic gastroenteritis, Crohn's disease, connective tissue) may cause esophageal eosinophilia and esophageal symptoms were excluded.
2.2 New active ingredient in eosinophilic esophagitis Eotaxin-3, a potent eosinophil chemotherapy, has been shown to be elevated (>50-fold) in esophageal biopsies from Patients with eosinophilic esophagitis compared with controls and eotaxin-3 was able to pull eosinophils into the esophagus. To understand the dynamics behind the regulation of eotaxin-3, a brief discussion of immune system activation is required. Every day, we ingest millions of antigens capable of triggering an immune response.
If one of these antigens receives the attention of the antigen presenting cell and the cell presents the antigen appropriately, the immune system can be activated and this can stimulate the immune system. differentiation of CD4+ T cells that have not been successful into Th1 or Th2 cells. Th2 cells secrete cytokines such as interleukin (IL)-5, IL-4, and IL-13, and overproduction of Th2 cells is characteristic of a number of allergic disorders, including esophagitis eosinophils. In human esophageal epithelial cells cultured in vitro, the Th2 cytokines IL-4 and IL-13 have been shown to stimulate production and secretion of eotaxin-3.
Thus, these data suggest that the pathogenesis of eosinophilic esophagitis begins in a genetically susceptible individual, to whom certain food allergens activate the esophagitis. immune system by binding to antigen-presenting cells that, in genetically susceptible humans, induce a Th2 response to Th2 production of cytokines such as IL-5, IL-4, and IL-13. IL-5 activates eosinophils residing in the bone marrow while IL-13 and IL-4 stimulate the production of eotaxin-3 by esophageal epithelial cells. Eotaxin-3 is a potent chemotherapeutic agent that induces activated eosinophils to reach the esophagus and eosinophils to cause epithelial damage by their degradation products. (Figure 1) Thus, this is a plausible model for the pathogenesis of eosinophilic esophagitis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3-20.e6; quiz 21-2. Rhonda F. Souza, Eosinophilic Esophagitis: When to Suspect and Why to Treat with Proton Pump Inhibitors, Dispatches from the guild conference, series
19, practicalgastro.