This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalThere are no standard guidelines for the management of ectopic gastric mucosal structures other than the clinical pathology classification system of Von Rahden et al., which aims to regulate management but is literature-based. limit.
1.Treatment and screening of ectopic gastric mucosa A thorough collaboration between disciplines (otolaryngologists, respiratory doctors, endocrinologists, gastroenterologists and psychiatrists) should be developed. psychiatry) to increase the effectiveness of diagnosing ectopic gastric mucosal structures in patients with unexplained extraesophageal symptoms.
Symptoms and their response to treatment may depend on many factors such as the type of ectopic gastric mucosal structure, H. pylori colonization and ectopic gastric mucosal structural factors extraesophageal, but further studies are needed to draw firm conclusions.
2. Is endoscopic re-evaluation of gastric mucosa ectopic? In the future, focus should be on patient reassurance and routine use of virtual staining of the proximal esophagus to guide appropriate biopsy sampling from gastric mucosa-like mucosa. misplaced thick. Another concern is whether repeat endoscopy is necessary after identification of an ectopic gastric mucosal structure. Currently, and likely due to its position as an underdiagnosed entity, there are no consensus guidelines for the management and monitoring of ectopic gastric mucosal structures.
As no relationship has been demonstrated between histopathology and clinical symptoms of ectopic gastric mucosal structures, symptomatic patients should be treated and considered for endoscopic reevaluation when Suspected other complications of ectopic gastric mucosa. In selected cases, such as patients at high risk for cancer or symptomatic patients, the elderly, or smokers, ectopic gastric mucosal structures should be evaluated systematically and Thoroughly described with endoscopic diagnosis and the patient should be considered for surveillance. Von Rahnen's classification used in conjunction with the NBI description may be included in the endoscopic report to improve awareness of any potential progression of the lesion at subsequent evaluation.
3. What drug should be treated in symptomatic patients? When a follow-up visit is scheduled, the patient may be sedated during the second evaluation for a better examination or a more accurate biopsy sample. A minimum of two biopsies should be performed depending on the size of the cervical esophageal mucosa or suspected precancerous lesion rather than ectopic gastric mucosa. An uncomplicated ectopic gastric mucosal structure suggests a similar treatment attitude for functional dyspepsia or non-erosive reflux disease. A differential diagnosis is required to determine which patients would benefit from alternative strategies. Since episodes of acid secretion are independent of a possible cause of symptoms, PPIs and/or antacids combined with psychological reassurance should be the initial treatment of choice for symptomatic patients. If the patient is anxious, low-dose anxiolytics can be used.

4. Duration of PPI Antisecretory Drugs The duration of PPI use is not well defined, but the authors have determined that therapy sessions are either “decreasing” or “increasing” for 4-8 weeks, similar to GERD treatment, followed by on-demand PPIs can be effectively applied. If there are relapses despite high-dose PPIs, supplementing an H2-receptor antagonist in the evening with a PPI in the morning may prevent the breakthrough of nocturnal acid secretion. Of course, the Future studies and more data are needed to demonstrate the effectiveness of this strategy. However, continuous and long-term use of both PPIs and H2 blockers is discouraged to avoid the development of resistance, acid reflux, and adverse events. Long-term PPI use also raises the question of whether it might affect the development of the metaplastic mucosa of the metaplastic or atrophic intestine. Interestingly, one study reported that lesions decreased in size after a course of 20 mg PPIs twice daily.
5. Should H.Pylori test in ectopic gastric mucosal structure? Similar gastric histological changes (inflammation, metaplasia, atrophic dysplasia and even adenocarcinoma of gastric mucosal structures ectopic with H. pylori invasion) have been reported. Although there are insufficient data to recommend testing for and to rule out H. pylori infection in patients with laryngopharyngeal reflux, the authors suggest that endoscopy physicians consider looking for gastric mucosal structures. ectopic in the cervical esophagus.
Then, a rapid urease test from ectopic gastric mucosa may be considered to determine the presence of H. pylori in patients with unexplained persistent dysphagia or dyspepsia. despite PPI treatment and absence of H. pylori. - positive gastritis , or the decision to continue treatment in patients with persistent dyspepsia after previous gastric H. pylori eradication . In both stomach and ectopic mucosa infected with H. pylori, eradication problems can also be considered, such as different susceptibility and resistance to antibiotics.
6. Role of argon or radiofrequency ablation of ectopic gastric mucosal structures In symptomatic patients with typical aspects of ectopic gastric mucosal structures unresponsive to PPIs , endoscopic therapy, such as argon ablation or radiofrequency ablation, has also been reported to be safe and effective. However, in the opinion of the authors, clinical management should be kept as non-invasive as possible as long as there are no adverse outcomes, complications or any suspicion of cancer. Endoscopic management is not only technically challenging due to the typical location of ectopic gastric mucosal structures proximal to the esophagus, but can also be available only in specialized centers.
7. Treatment of esophageal stricture and septum due to ectopic gastric mucosal structures. esophageal strictures and diaphragms can be managed with serial balloon dilation and biopsy to rule out malignancy. High-dose PPIs combined with endoscopic thermal ablation of lesions lead to persistent dysphagia in the presence of narrow ectopic gastric mucosa and even mucosal restoration with normal squamous epithelium. Endoscopic mucosal resection (EMR), argon ablation (APC), or surgical resection have also been used to successfully treat ectopic gastric mucosal dysplasia or early cancer. although the routine use of these strategies in this context has not been studied.
8. Is there a need to intervene in the gastric mucosal structure of large size or protruding form? Other issues such as raised surface or scale of ectopic gastric mucosa should be considered before deciding which strategy is most appropriate. For example, specialists generally do not re-intervention in patients with large ectopic gastric mucosal structures in interventional APC trials that have been conducted previously to exclude the possibility of narrow scar formation. Furthermore, large areas of excised tissue and multiple lesions are independent predictors for esophageal stricture formation.
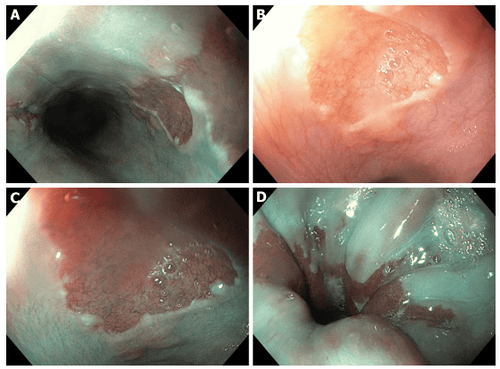
Three ectopic gastric mucosal structures in the cervical esophagus, with a symmetrical distribution, in middle-aged women with a history of uterine cancer, presenting with complaints of reflux and sensation of swallowing choking. Detailed images in (B) white light endoscopy and (C) NBI narrowband imaging. D: Irregular Z-line in the same patient suggests concomitant gastroesophageal reflux disease.
In contrast, Kristo et al. recently reported an 80% complete histological and gross cure rate after 2 radiofrequency ablations with demonstrations of dysphagia and quality of life. did not have any major or serious side effects after about 2 -years of follow-up. Involvement of ectopic gastric mucosa in esophageal pathology may eventually become as common as Barrett's esophagus, which will spur new technologies such as hybrid-APC that can improve intervention treatment intervention for selected cases of large ectopic gastric mucosal structures in the future. Confocal laser endoscopy may allow in vivo histological examination for flat lesions in the cervical esophagus to avoid some unnecessary biopsies and to further direct any EMR or lower laparoscopy. any mucosa.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Raine CH . Ectopic gastric mucosa in the upper esophagus as a cause of dysphagia. Ann Otol Rhinol Laryngol . 1983; 92 :65-66. [PubMed] [DOI] Truong LD, Stroehlein JR, McKechnie JC. Gastric heterotopia of the proximal esophagus: a report of four cases detected by endoscopy and review of literature. Am J Gastroenterol . 1986; 81:1162-1166. [PubMed] Akbayir N , Alkim C, Erdem L, Sökmen HM, Sungun A, Başak T, Turgut S, Mungan Z. Heterotopic gastric mucosa in the cervical esophagus (inlet patch): endoscopic prevalence, histological and clinical characteristics. J Gastroenterol Hepatol . 2004; 19:891-896. [PubMed] [DOI] Borhan-Manesh F , Farnum JB. Incidence of heterotopic gastric mucosa in the upper oesophagus. Gut . 1991; 32 :968-972. [PubMed] [DOI] Tang P , McKinley MJ, Sporrer M, Kahn E. Inlet patch: prevalence, histologic type, and association with esophagitis, Barrett esophagus, and antritis. Arch Pathol Lab Med . 2004; 128 :444-447. [PubMed] [DOI] Adriana Ciocalteu, Petrica Popa, Issues and controversies in esophageal inlet patch, World J Gastroenterol. Aug 14, 2019; 25(30): 4061-4073