This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
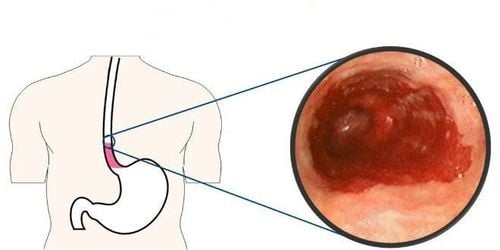
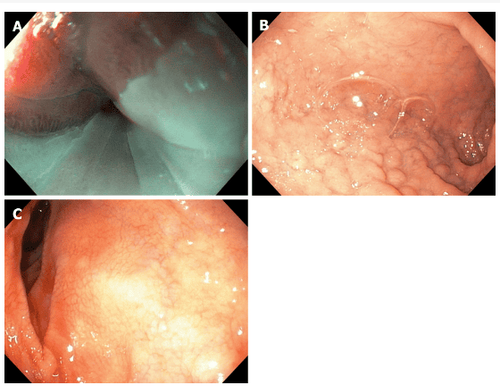
In isolated cases, there have been reports of complications including bleeding, ulceration, stricture, perforation and fistula, and subcutaneous abscess. In a small series of cases, the detection of an ectopic gastric mucosal membrane or ring suggests the pathogenesis of an acid-induced lesion. Importantly, H. pylori colonization can exacerbate these complications.
1. Complications of ectopic gastric mucosal structure
Other studies have also described cases of food effects involving strict rings or rings associated with ectopic gastric mucosal structures.
Concurrent findings of ectopic gastric mucosal structures in patients with inflammatory bowel disease, celiac disease, neurofibromatosis, or nevus syndrome may be incidental.
Recently, an isolated case of eosinophilic gastritis was described with involvement of ectopic gastric mucosal polypoid structures and it was reported that dysphagia and hoarseness resolved. decided after resection. It should also be noted that the first reported case of an esophageal xanthoma in an ectopic gastric mucosal structure in the cervical esophagus can be interpreted as a chronic lesion of an ectopic gastric mucosal structure.
2. Ectopic gastric mucosa structure - Congenital or acquired structure
The incidence of ectopic gastric mucosal structures is higher in the pediatric population, and immunohistochemical studies showing embryonic origin support the hypothesis that it is a congenital condition. During normal embryonic development, the squamous cell epithelium of the esophagus is replaced by a columnar epithelium starting from the middle esophagus to the cervical esophagus. However, areas of persistent columnar lining that result from incomplete squamous epithelialization can differentiate into ectopic gastric mucosal structures. Interestingly, a lower prevalence has been reported in older populations and some authors have suggested that ectopic gastric mucosal structures may regress with age.
3. Does intestinal metaplasia occur on ectopic gastric mucosal structures?
Going beyond this classical theory, the hypothesis that long-term acid reflux can lead to the development of ectopic gastric mucosal structures with intestinal metaplasia in the upper esophagus seems less credible because histologically Rarely shows any other intestinal metaplasia on ectopic gastric mucosal structures. Thus, the entry pathway may be congenital and may be predisposed to several conditions due to its primary histology and subsequently to be further influenced by other cumulative factors such as H. pylori colonization, and concomitant have gastroesophageal reflux disease (GERD) or Barrett's esophagus.
The authors recommend that the association between ectopic gastric mucosal structure and GERD be investigated in patients without synchronous Barrett's esophagus. Furthermore, care should be taken not to overestimate the association between ectopic gastric mucosal structure and GERD due to the upper acid reflux produced by the gastric foreign body.
4. Ectopic gastric mucosa and functional digestive disorders
Injuries to the cervical esophagus should be recognized and addressed, especially in the absence of other upper tract lesions that could account for the patient's complaints, and these steps should be taken. before diagnosing functional dyspepsia or non-erosive reflux disease. Patients who have been diagnosed with a potentially functional gastrointestinal disorder may be frustrated by the failure to find a cause for their condition. This condition can lead to a vicious cycle of anxiety.
Furthermore, simply explaining to patients that harmless ectopic gastric mucosal structures in their esophagus may be causing their symptoms can help better manage their condition through effective placebo response. Psychological discomfort is common and the pathophysiology of persistent functional dyspepsia is not well understood. However, persistent choking sensation can also originate from pressure on the upper esophageal sphincter resulting from an ectopic gastric mucosal structure that is easily irritated or from reflex esophageal sphincter contraction. due to a respiratory protective mechanism, possibly related to reflux.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Raine CH . Ectopic gastric mucosa in the upper esophagus as a cause of dysphagia. Ann Otol Rhinol Laryngol . 1983; 92 :65-66. [PubMed] [DOI] Truong LD, Stroehlein JR, McKechnie JC. Gastric heterotopia of the proximal esophagus: a report of four cases detected by endoscopy and review of literature. Am J Gastroenterol . 1986; 81:1162-1166. [PubMed] Akbayir N , Alkim C, Erdem L, Sökmen HM, Sungun A, Başak T, Turgut S, Mungan Z. Heterotopic gastric mucosa in the cervical esophagus (inlet patch): endoscopic prevalence, histological and clinical characteristics. J Gastroenterol Hepatol . 2004; 19:891-896. [PubMed] [DOI] Borhan-Manesh F , Farnum JB. Incidence of heterotopic gastric mucosa in the upper oesophagus. Gut . 1991; 32 :968-972. [PubMed] [DOI] Tang P , McKinley MJ, Sporrer M, Kahn E. Inlet patch: prevalence, histologic type, and association with esophagitis, Barrett esophagus, and antritis. Arch Pathol Lab Med . 2004; 128 :444-447. [PubMed] [DOI] Adriana Ciocalteu, Petrica Popa, Issues and controversies in esophageal inlet patch, World J Gastroenterol. Aug 14, 2019; 25(30): 4061-4073