This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalH. pylori density and mucosal type were the only predictors of active inflammation in ectopic gastric mucosal structures and a higher likelihood of inflammation in patients with H. pylori infection. active in the mucosa other than the ectopic gastric mucosal structure.
1. Esophageal motility disorders and ectopic gastric mucosa
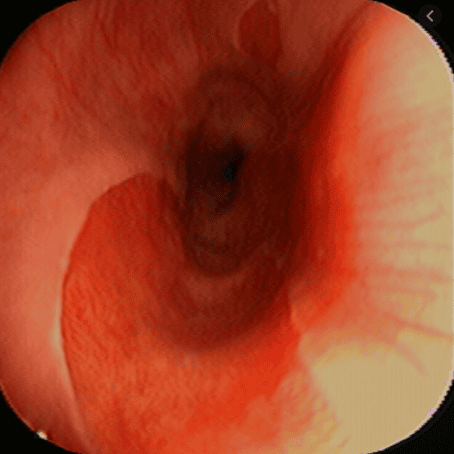
There has been considerable debate about synchronous motility disorders, and Korkut et al. have shown that there is esophageal motility dysfunction in some patients with ectopic gastric mucosal structures based on barometer and 24-hour dual-probe pH study, may also be causative for symptomatic patients without other gastrointestinal disturbances.Rosztoczy et al. reported prolonged acid exposure in both the cervical and distal esophagus, longer duration of bile reflux exposure in the distal esophagus, prolonged relaxation, and decreased parietal wave amplitude. movement, and decreased lower esophageal sphincter pressure may be other factors contributing to abnormal motor function in these patients.
Another study speculates that mucus secretion rather than acid production may be the cause of symptoms in patients with dysphagia unresponsive to PPI therapy. In these few patients, histopathological examination revealed only the presence of cardiac mucosa.
2. Ectopic gastric mucosal structure and accompanying non-neoplastic lesions
The association of ectopic gastric mucosal structure with Barrett's esophagus and gastric lesions such as Helicobacter pylori-associated gastritis (H. Pylori) has been debated in many studies.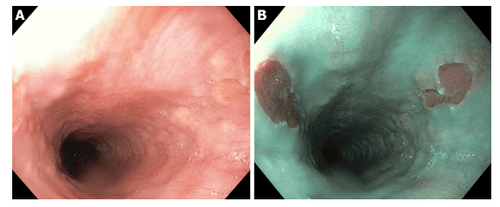
3. Ectopic gastric mucosa and pathogenicity of H.Pylori
In contrast, another study showed that ectopic gastric mucosal structural type did not affect the rate of H. pylori colonization and found that H. pylori density and mucosal type were factors. The only predictor of active inflammation in ectopic gastric mucosal structures and a higher likelihood of inflammation in patients with active H. PYLORI infection in mucosa other than mucosal structures misplaced stomach.In 2010, Alagozlu et al found that ectopic gastric mucosal structures were positive for H. pylori in 23.5% of patients with a higher localization rate in female patients than in male patients ( P < 0.05), and further showed that the sensation of choking is a symptom persistence. Interestingly, this study found that H. pylori was most prevalent in the muscularis mucosa (81.2%) and that synchronous H. pylori gastritis was present in all patients with structural infection. misplaced gastric mucosa. Size ranges have been reported, from 5 to 32 mm and from 10% to 30% of the circumference of the proximal esophagus, but they did not determine whether the increased localization rate was size dependent.
4. Size of ectopic gastric mucosa and relationship to clinical symptom severity
However, several reports have shown that the size of the ectopic gastric mucosa may be associated with symptoms (correlation with severity of dysphagia) and hypothesized that it may be a acid-secreting function or by narrow scar formation at the distal end of the ectopic gastric mucosal structure.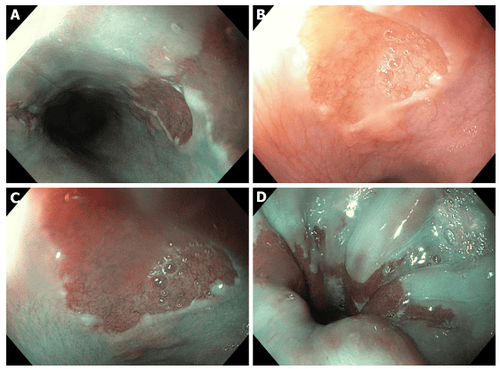
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferenceRaine CH. Ectopic gastric mucosa in the upper esophagus as a cause of dysphagia. Ann Otol Rhinol Laryngol. 1983; 92 :65-66. [PubMed] [DOI] Truong LD, Stroehlein JR, McKechnie JC. Gastric heterotopia of the proximal esophagus: a report of four cases detected by endoscopy and review of literature. AmJ Gastroenterol. 1986; 81:1162-1166. [PubMed] Akbayir N , Alkim C, Erdem L, Sökmen HM, Sungun A, Başak T, Turgut S, Mungan Z. Heterotopic gastric mucosa in the cervical esophagus (inlet patch): endoscopic prevalence, histological and clinical characteristics. J Gastroenterol Hepatol. 2004; 19:891-896. [PubMed] [DOI] Borhan-Manesh F , Farnum JB. Incidence of heterotopic gastric mucosa in the upper oesophagus. Gut. 1991; 32 :968-972. [PubMed] [DOI] Tang P , McKinley MJ, Sporrer M, Kahn E. Inlet patch: prevalence, histologic type, and association with esophagitis, Barrett esophagus, and antritis. Arch Pathol Lab Med. 2004; 128 :444-447. [PubMed] [DOI] Adriana Ciocalteu, Petrica Popa, Issues and controversies in esophageal inlet patch, World J Gastroenterol. Aug 14, 2019; 25(30): 4061-4073














