Article written by Dr. Tran Quynh Trang, MSc, MD, Department of Laboratory Medicine – Vinmec Times City International General Hospital
The complement system consists of more than 20 different serum proteins that contribute to the body’s defense through various pathways. C3 and C4 are the two main components of the complement system and are used to assess its function and role in immune responses, infections, and autoimmune diseases.
The term "complement" refers to a heat-labile serum component capable of lysing bacteria and protecting the body through different mechanisms.
Complement can opsonize bacteria to enhance phagocytosis, recruit and activate various cells including polymorphonuclear leukocytes and macrophages, regulate antibody responses, and assist in clearing immune complexes and apoptotic cells.
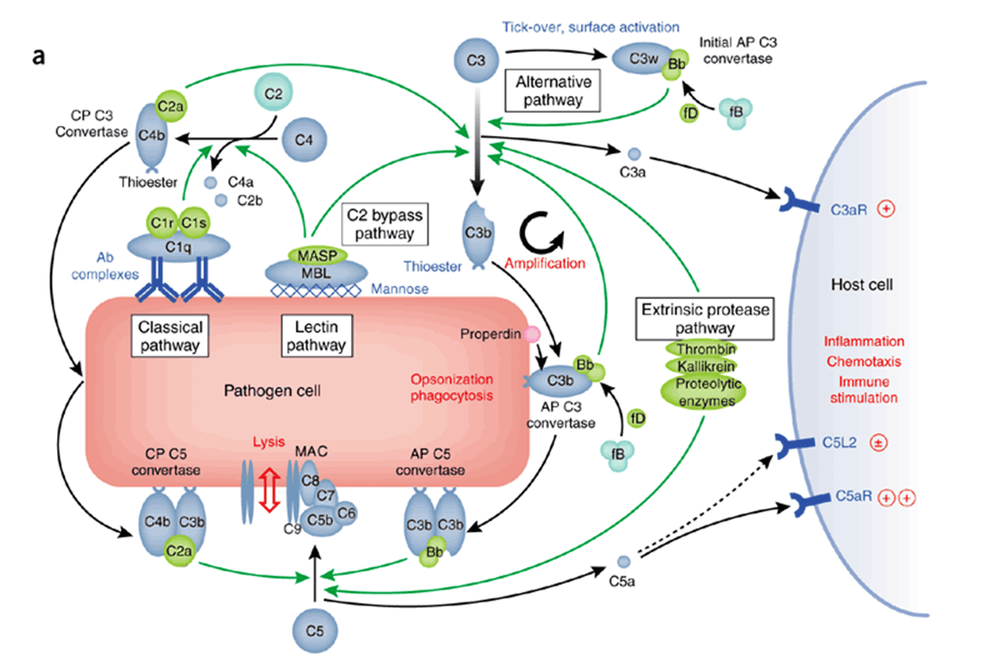
The complement system comprises over 20 different serum proteins produced by various cells, including liver cells, macrophages, and intestinal epithelial cells.
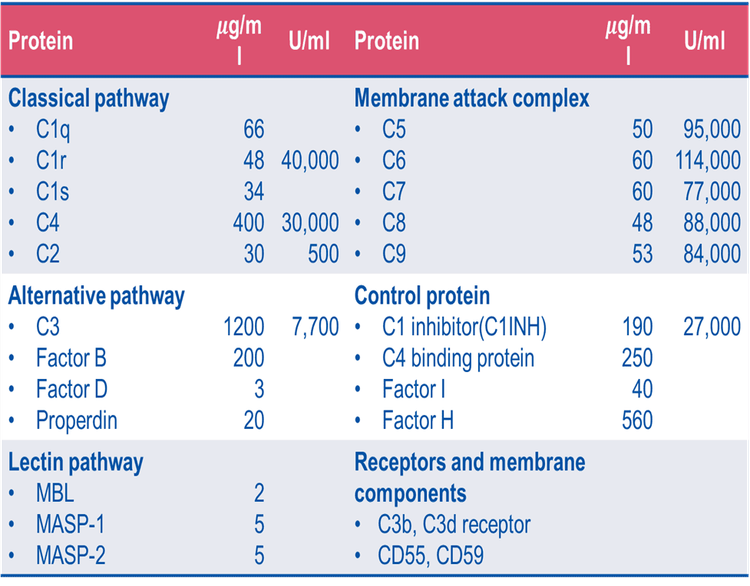
Certain complement proteins bind to immunoglobulins or other cell membrane components. Many other complement components exist in proenzyme form and, once activated, cleave one or more additional complement proteins. Cleaving these complement proteins generates fragments that can activate cells, increase vascular permeability, or opsonize bacteria.
Complement activation occurs through four pathways: the classical pathway, the lectin pathway, the alternative pathway, and the membrane attack complex (MAC) pathway. Regardless of the activation pathway, the end product is a protein complex capable of destroying the target cell membrane.
To evaluate the function of the complement system and its role in immune responses, infections, or autoimmune diseases, C3 and C4 are typically quantified as key components.
Although genetic C3 deficiency is extremely rare, deficiencies in other complement components, while still uncommon, may result in low C3 levels. Genetic C4 deficiency is rarely detected.
Quantification of C3 and C4 helps to:
• Detect causes of disorders in kidney tissue, joints, connective tissue, glomerulonephritis, and vasculitis.
• Identify causes of immunodeficiency related to recurrent infections.
Normal C4 Levels: 20–50 mg/dl
Increased C4 levels are seen in: cancer, rheumatoid arthritis, rheumatoid spondylitis
Decreased C4 levels indicate immune complex-related diseases. These are most commonly found in: Active systemic lupus erythematosus (SLE), rheumatoid vasculitis (but not uncomplicated rheumatoid arthritis, where C4 levels are usually normal), chronic active hepatitis, congenital C4 deficiency, hereditary angioedema
Normal C3 Levels: 90–180 mg/dl
Values up to twice the upper limit may be observed during acute phases.
Increased C3 levels are found in: Acute rheumatism, rheumatoid arthritis, cancer
Decreased C3 levels are seen in: SLE, glomerulonephritis, septicemia. Low C3 levels combined with low C4 levels suggest activation of the classical complement pathway, commonly found in active SLE. Low C3 levels with normal C4 levels suggest activation of the alternative pathway, indicating infectious diseases or renal factor activity.
Although C3 levels remain low in some long-term SLE patients, this does not necessarily indicate active disease. A sudden decrease in C3 levels often signals disease exacerbation and an increased risk of kidney damage.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.












