This is an automatically translated article.
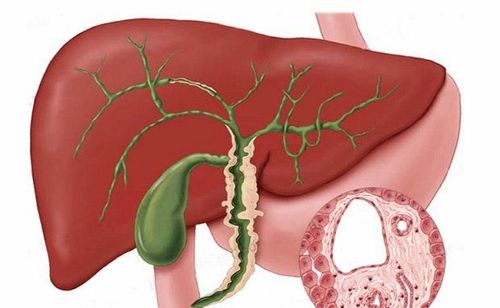
The interaction between bile acids and the gut microbiota is implicated in the pathophysiology of many intestinal and gastrointestinal diseases, especially cholestatic liver disease. In particular, the progression of autoimmune cholestatic liver diseases also affects the composition of the gut microbiota, exacerbating the development of cholestasis in this interactive cycle.1. Overview
Bile acids are essential signaling molecules for bidirectional regulation between the liver and the gut, which are mainly activated by the following two signaling pathways:
Bind the signaling molecule to the bile acid receptor 1 to the G protein (GPBAR1 or TGR5) Activates the expression of xanesoid activating receptor X (FXR). The above two pathways control energy metabolism balance, modulate fatty and inflammatory responses in the liver, influence the composition of the gut microbiota by shaping intestinal immunity, and some antibacterial properties of endogenous peptides. Therefore, the use of bile acids as signaling molecules by the gut microbiota may play a role in the pathophysiology of liver diseases. Better characterization of the specific active sites of the gut microbiota and bile acids in different signaling pathways in liver diseases could lay the groundwork for novel therapies targeting bile acids. The interaction between bile acids and the gut microbiota has been implicated in the pathophysiology of many intestinal and intestinal diseases, especially liver diseases. As an essential mediator of the gut-liver junction, bile acids modulate host-specific metabolic pathways and modulate inflammatory responses through the farnesoid-activated receptor, the associated bile acid receptor. with G1 protein. Several clinical trials have demonstrated the signaling effects of bile acids in the setting of liver disease.
2. Cholestatic liver disease and bile acids
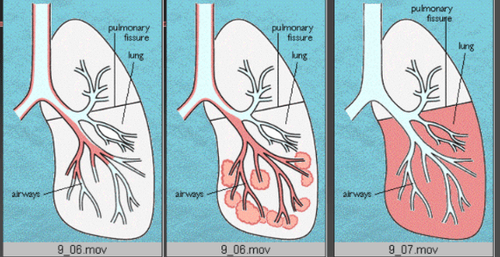
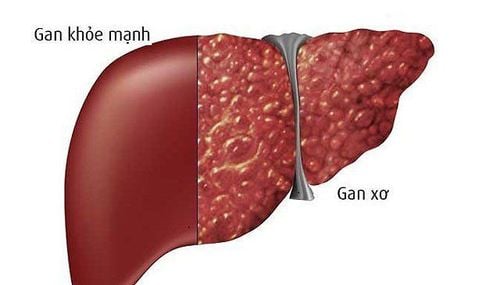
Chronic cholestasis can lead to liver damage by affecting the expression levels of nuclear receptors and bile acid transporters. Hydrophobic bile acids can cause liver cell damage. Bile salts can induce apoptosis at concentrations of 50-200 μmol/L, induce proinflammatory responses at concentrations of 200 μmol/L and cell necrosis at concentrations of 200-2000 μmol/L. Autoimmune cholestatic liver disease also affects the composition of the gut microbiota, exacerbating the development of cholestasis in this interactive cycle.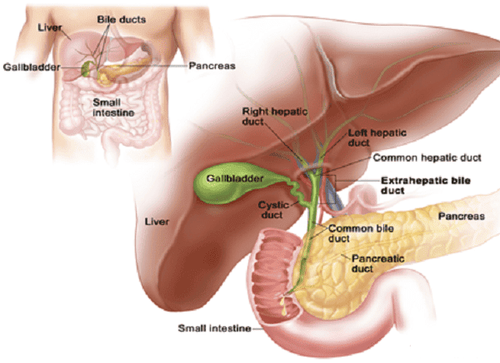
Sự tiến triển của các bệnh gan ứ mật tự miễn cũng ảnh hưởng đến thành phần của hệ vi sinh vật đường ruột
4. Role of Bile Acid in Previous Studies In previous studies, bile acid has been implicated as a tissue-damaging factor that promotes inflammation due to its chemical properties. Its detergent effect can destroy cell membranes and mitochondria. Overall, there are three important pathways of bile acid-induced cytotoxicity:
Oxidative stress in the endoplasmic reticulum and mitochondria; Direct activation of death receptors Traill2 and Fas; Lysates the plasma membrane of hepatocytes. As such, the accumulation of hydrophobic bile acids is the leading cause of intrahepatic cholestasis. However, a recent paper suggested that two derivatives of lithocholic acid (LCA) (isoalloLCA and 3-oxolCA) may influence the adaptive immune response by regulating helper T cell differentiation. (Th)17 and regulatory T (Treg) cells. They are mutually limited in function, and their ratio variation has a decisive role in the pathogenesis and clinical prognosis of autoimmune and inflammatory diseases.
Many studies have shown an imbalance between Th17 and Treg cells in PBC patients. These patients had a defective CD8+ Treg cell subset and preferentially activated Th17 cells. IsoalloLCA can promote Treg cell differentiation by increasing mitochondrial reactive oxygen species synthesis and expression of H3K27ac in the Foxp3 promoter region under the induction of TGF-β signaling. Another LCA derivative, 3-oxoLCA, inhibits the differentiation of Th17 cells, and IL-17a expression is significantly reduced, thereby inhibiting the inflammatory process.
The results demonstrated that, LCA derivatives (isoalloLCA and 3-oxoLCA) can regulate the balance between Th17 and Treg cells, which has great significance in the treatment of cholestatic liver diseases. Furthermore, isoalloLCA and 3-oxoLCA are expected to be used to treat autoimmune or inflammatory diseases caused by Th17/Treg cell imbalance in the future.
5. Bile acids in the regulation of the adaptive and innate immune system through the enteric-bile acid-liver triangle Among them, ursodeoxycholic acid (UDCA) is currently the only drug approved to treat PBC. It can effectively reduce the retention of toxic bile acids in liver cells and soothe liver damage. However, UDCA has limited efficacy in cholestatic liver disease, and some patients cannot tolerate the adverse effects of UDCA (such as gastrointestinal symptoms).
Developing effective medical therapy for cholestatic liver disease is urgently important. 24-norursodeoxycholic acid (norUDCA), a C23 homolog of UDCA with shortened side chains, has potent anti-fibrotic, anti-venous and anti-inflammatory properties. In a phase II clinical study, 12 weeks of treatment with norUDCA significantly reduced serum alkaline phosphatase levels in PSC patients. A multicenter randomized controlled trial evaluating the efficacy and safety of norUDCA (500 mg/day, 1000 mg/day, or 1500 mg/day) compared with placebo in PSC patients. NorUDCA was shown to have the same excellent safety profile as placebo.
Another bile acid, OCA - an FXR agonist, has shown potential benefits for PBC. It has about 100 times greater FXR activation effect than CDCA. OCA protects hepatocytes from the toxic effects of bile acids by activating the FXR receptor, which reduces bile acid synthesis and improves bile secretion. In addition to the effect of FXR on bile acid homeostasis, OCA monotherapy can improve the secretion of IgM and tumor necrosis factor-α as well as have direct immunomodulatory, anti-fibrotic, and anti-fibrotic effects. Anti-inflammatory. In clinical trials, OCA monotherapy significantly reduced baseline alkaline phosphatase and bilirubin levels compared with placebo. However, OCA treatment caused a dose-related increase in itching.
In conclusion, OCA may represent a new treatment option for PBC patients who cannot tolerate UDCA. Exploring new bile acids and understanding how best to use different bile acids can help develop new treatments for cholestatic liver disease.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Shao JW, Ge TT, Chen SZ, Wang G, Yang Q, Huang CH, Xu LC, Chen Z. Role of bile acids in liver diseases mediated by the gut microbiome. World J Gastroenterol 2021; 27(22): 3010-3021 [DOI: 10.3748/wjg.v27.i22.3010]