This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Previous studies have shown that gut microbiota changes or dysbacteriosis in patients with chronic liver disease or cirrhosis are often accompanied by significant reductions in total bile acids and rates secondary bile acids/primary bile acids.
1. Role of Bile Acid
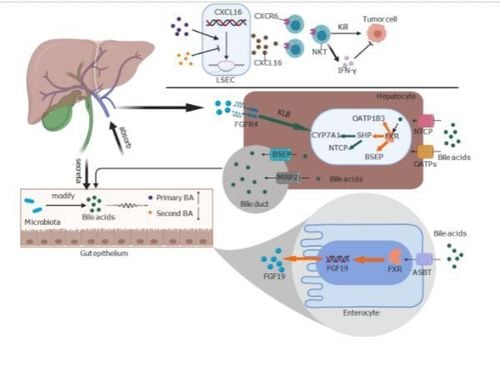
Bile acids are essential signaling molecules for bidirectional regulation between the liver and the gut, mainly activated by the following two signaling pathways:
Binding of the signaling molecule to the bile acid receptor 1 to G protein (GPBAR1 or TGR5) Activates the expression of xanesoid activator X receptor (FXR). The above two pathways control energy-metabolic balance, modulate hepatic steatosis and inflammatory responses, and influence the composition of the gut microbiota by shaping intestinal immunity and a antimicrobial properties of endogenous peptides. Therefore, the use of bile acids as signaling molecules by the gut microbiota may play a role in the pathophysiology of liver diseases.
In fact, studies have demonstrated a positive correlation of Enterobacteriaceae with endotoxin inflammation and fecal CDCA concentrations. These metabolites are derived from oxidative stress and metabolism of ammonia and aromatic amino acids are positively related to the Porphyromonadaceae and Enterobacteriaceae families as well as closely related to the occurrence of hepatic encephalopathy.
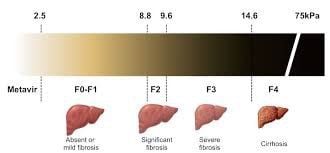
Kakiyama et al. suggested that intestinal microbiota disturbance in cirrhotic patients is partly due to decreased intestinal bile acid concentration. For example, a decrease in the number of 7α-dehydroxylated bile acids bacteria is due to a decrease in the level of the main bile acid in the colon, which serves as an energy source. Decreased levels of bile acids entering the small intestine can lead to bacterial overgrowth and protein metabolism, and cause release of metabolic markers as well as increased liver inflammation. Hepatitis activates a positive feedback mechanism, which can further inhibit bile acid synthesis. The size and composition of the bile acid pool can significantly modulate the gut microbiota structure and serve as an indicator of the severity of liver diseases. In summary, the balance of the liver - acid - bile - intestinal microbial axis is essential for human health and against liver fibrosis.
3. Increasing the DCA/cholic acid ratio in cirrhotic patients can improve toxic metabolites from the gut microbiota DCA is the most effective antibacterial in bile acids, produced by 7α bacteria. -dehydroxylation of bile acids. Studies have shown that increasing the DCA/cholic acid ratio in cirrhotic patients can improve toxic metabolites from the gut microbiota, increase the incidence of endotoxin and hepatic encephalopathy. , which may be involved in the destruction of the intestinal mucosal barrier by DCA. Compared with DCA that exacerbated the barrier dysfunction, LCA had much less destructive effect on the gut microbiota due to its insolubility in water and ease of excretion in faeces. TGR5 is a membrane receptor that can be activated by a variety of bile acids, of which LCA is its strongest natural agonist. In the study by Guo et al., LCA inhibits the activation of the Nod-like receptor 3 protein via the TGR5-cAMP-protein kinase A axis, which significantly inhibits caspase-1 maturation and IL-B secretion . or IL-18. In addition, LCA was also shown to reduce lipopolysaccharide-induced release of proinflammatory cytokines and macrophage phagocytosis activity through TGR5, thereby inhibiting the hepatitis process.
Recent studies have shown that two different metabolites of LCA can also control host immune responses in both humans and mice. In clinical studies, the fecal LCA content of patients with advanced cirrhosis was significantly lower than that of patients with early-stage cirrhosis. Previous studies have focused on the cytotoxicity of bile acids. However, recent studies have revealed the anti-inflammatory and immunomodulatory effects of bile acids. There is growing evidence that bile acids are a potential therapeutic target against inflammatory diseases. Appropriate elevation of bile acid levels in cirrhotic patients may suppress liver inflammation and ameliorate liver fibrosis, which merits further discussion.
4. Conclusion Many studies in recent decades have shown that the function of bile acids goes beyond the function of “digestive surfactants”. At the host level, there is a clear relationship between bile acid signaling and innate immunity in the liver and gut. In other words, bile acids are the cornerstone of the immune axis between the liver and the gut microbiota. As a mediator in the gut-hepatic axis, bile acids can modulate inflammation, host metabolism, and innate immunity, which are effective therapeutic targets in the setting of various liver diseases. However, most contemporary studies on bile acids are based on transgenic mouse models, while the immune system, bile acid metabolism, and gut microbiota of mice are very different from those of humans.
Recent clinical trials of FXR agonists have yielded promising results. Preclinical data suggest that gut microbiota bile acid metabolism is also a potential therapeutic target. Changes in the gut microbiome to regulate the composition of bile acids may improve liver health through the use of antibiotics, probiotics, prebiotics, and fecal bacterial cultures. The complex interactions between bile acids and the host microbiota in the hepatobiliary axis are only just beginning to be understood. Clinical trials and further studies may help identify the different roles of bile acids in healthy subjects and patients with liver disease, allowing them to be optimally used as potential therapeutic targets. power.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Shao JW, Ge TT, Chen SZ, Wang G, Yang Q, Huang CH, Xu LC, Chen Z. Role of bile acids in liver diseases mediated by the gut microbiome. World J Gastroenterol 2021; 27(22): 3010-3021 [DOI: 10.3748/wjg.v27.i22.3010]