Cirrhosis is a serious chronic liver disease that can result in severe complications, including death without prompt diagnosis and management. What factor determines the life expectancy of end stage liver disease, and what can be done to extend the time patients have?
1. Stages of liver disease
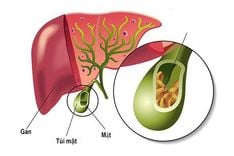
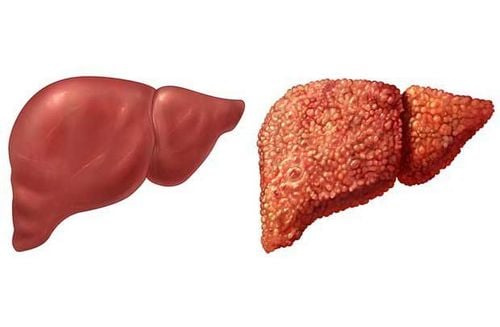
The liver is the largest abdominal organ of the human body. Liver cirrhosis occurs as liver tissue is gradually replaced by scar tissue, resulting in many complications, one of which being loss of liver function, either temporary or permanent.
Based on the extent of liver damage, cirrhosis is classified into 4 stages F1-F4, with F4 being end stage liver disease and associated with high mortality.
A diagnosis of end stage liver disease indicates severe damage to the liver, with prominent scar tissue replacing liver tissue. As a result, most functions of the liver are greatly impaired at this point.
The prognosis for patients diagnosed with end stage liver disease is poor. However, each individual prognosis will differ greatly due to many factors, such as available treatment options, and tolerance of treatment.
Trắc nghiệm: Làm thế nào để bảo vệ lá gan khỏe mạnh?
Làm test trắc nghiệm kiểm tra hiểu biết về gan có thể giúp bạn nhận thức rõ vai trò quan trọng của gan, từ đó có các biện pháp bảo vệ gan để phòng ngừa bệnh tật.2. Life expectancy of liver cirrhosis
The severity of cirrhosis is characterized by symptoms of end stage liver disease, and associated complications. Statistically, up to 30% of end stage liver disease patients develop hemodynamic complications due to variceal bleeding. Furthermore, the mortality rate of first variceal bleed can be as high as 55%.
The most severe complication of end stage liver disease is liver cancer. So how long can a patient with end stage liver disease expect to live for? Under certain circumstances, liver transplantation can prolong life for a few more years. Death usually occurs in 24 months without appropriate medical intervention. However, many patients only live for about 6 months due to liver cancer.
To prevent complications, management of cirrhosis is of highest priority. At this point, there is no consensus on the most effective management for liver cirrhosis
For end stage liver disease, appropriate medical intervention can give patients 1-3 years of life. However, up to 50% of patients do not live past 12 months since diagnosis. Life expectancy depends on several factors, such as:
- the patient’s overall health
- Treatment options available
- Severity of complication(s)
3. Treatment options for end stage liver disease
Common treatments for end stage liver disease includes:
- Abdominal paracentesis
- Medications as per approved guidelines
- Liver transplantation
The first two are used for the purpose of relieving symptom severity and preventing further complications from developing.
Liver transplantation can eliminate existing scar tissue, and is generally considered the best prognostically for patients of end stage liver disease.
On a theoretical basis, liver transplantation can prolong life for up to 20 years, however, only 70% of recipients live past the 5-years mark.
Not all patients are suitable for liver transplantation. Patients must first meet all criteria required to be placed on a recipient list. The cost of liver transplantation remains high, making it not readily accessible for many.
For patients diagnosed with cirrhosis at the F4 stage, treatment of symptoms should be accompanied by measures to improve their immunity, such as:
- A balanced diet for the individual patient
- Limited intake of salt and fat
- Food items rich in vitamins, fiber, and antioxidants.
- Regular exercise as indicated by physician
- Avoiding physical exertion
- Taking medications as instructed by physician
- Avoid using medication for pain relief, supplementation, or herbal medication without first consulting the primary physician first.
Life expectancy of end stage liver disease can vary greatly due to many contributing factors. Most pivotal is the prompt diagnosis and treatment. Please visit a reputable healthcare facility if you identify any typical symptoms of cirrhosis.
Currently, Vinmec General Hospital provides screening tests for hepatobiliary function that can detect viral hepatitis, even before symptoms show. The comprehensive hepatobiliary screen includes the following:
- Liver function tests
- Bile function tests
- Early screening of liver cancer
- Blood tests: complete blood count; clotting factors, screening for viral hepatitis B & C.
- Evaluation of hepatobiliary function via ultrasound (including conditions that can cause/worsen liver function disorders)
- Analysis of lab values and rsks factors that involve the liver, and early screening for hepatobiliary malignancies.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.