This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
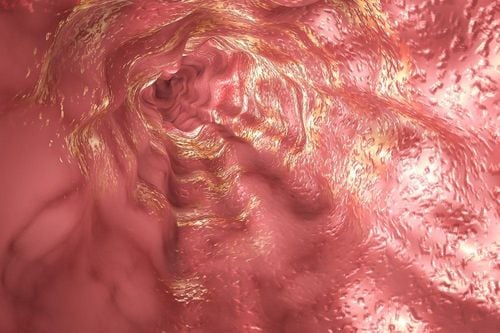
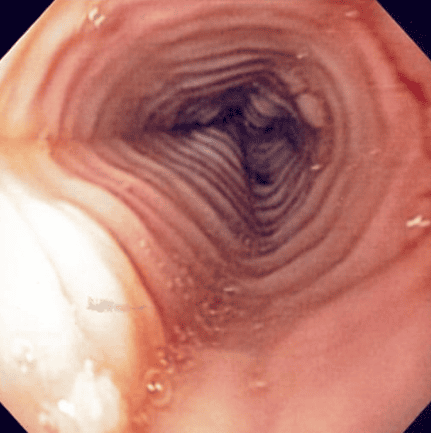
Eosinophilic esophagitis (eosinophilic esophagitis) is a chronic, immune-mediated disease caused by food allergens, presenting with symptoms of dysfunction oesophagitis and esophagitis predominated by eosinophils.
Recent consensus guidelines now include proton pump inhibitor therapy as an alternative first-line treatment. This review will provide an overview of when to suspect and how to diagnose eosinophilic esophagitis, the concepts surrounding the pathogenesis, and increased incidence of the newly discovered esophageal condition. recognize this, and discuss why proton pump inhibitors are currently being used as a first-line treatment strategy.
1. Overview of eosinophilic esophagitis
Eosinophilic esophagitis (EoE) is a chronic, immunological or antigenic esophageal disorder that is clinically characterized by symptoms of esophageal dysfunction and histologically by eosinophil infiltration in the esophageal epithelium. Eosinophilic esophagitis was rarely recognized prior to the 1990s. Current epidemiological data estimate that the prevalence of eosinophilic esophagitis is 50 to 100 cases per 100,000 fish. in the United States with the cost of diagnosing and treating this condition between $0.5 and $1.4 billion per year.This is quite amazing for a disease that was unknown only twenty years ago. Management of patients with eosinophilic esophagitis draws on the expertise of providers in the areas of primary care, gastroenterology, allergy and immunology, and nutrition. The length of time that a patient has undiagnosed and untreated eosinophilic esophagitis correlates significantly with the risk of esophageal stricture, a major complication of eosinophilic esophagitis. .
2. When to suspect and how to diagnose eosinophilic esophagitis?
Eosinophilic esophagitis affects children and adults of all ages of all races and ethnicities, with reports of eosinophilic esophagitis from countries around the world . Eosinophilic esophagitis affects both sexes but is male predominant by a factor of about 3 to 1.
Physicians should suspect eosinophilic esophagitis when patients present with symptoms of the disorder. esophageal function. Esophageal dysphagia is reported by 60-100% of patients with eosinophilic esophagitis and more than 25% of these patients have experienced regurgitation. Patients often complain of chest pain, heartburn, and upper abdominal pain. A history of allergic disease such as rhinitis, asthma, or atopic dermatitis is found in 50-60% of patients with eosinophilic esophagitis. In addition, a family history of eosinophilic esophagitis or dysphagia will further increase your clinical suspicion for eosinophilic esophagitis.
3. The role of factor Eotaxin-3
Eotaxin-3, a potent chemoattractant for eosinophils, was shown to be elevated (>50-fold) in esophageal biopsies from patients with eosinophilic esophagitis compared with the control group. control and eotaxin-3 can pull eosinophils into the esophagus. To understand the dynamics behind the regulation of eotaxin-3, a brief discussion of immune system activation is required. Every day, we ingest millions of antigens capable of triggering an immune response. If one of these antigens receives the attention of the antigen-presenting cell and the cell presents the antigen appropriately, the immune system can be activated and this can stimulate differentiation. The transformation of CD4+ T cells has not been successful into Th1 or Th2 cells. Th2 cells secrete cytokines such as interleukin (IL)-5, IL-4, and IL-13, and overproduction of Th2 cells is characteristic of a number of allergic disorders, including esophagitis eosinophils. In human esophageal epithelial cells cultured in vitro, the Th2 cytokines IL-4 and IL-13 have been shown to stimulate production and secretion of eotaxin-3.
4. Proposed hypothesis to explain the increased frequency of eosinophilic esophagitis
The hygiene hypothesis suggests that modern sanitary conditions lead to fewer bacterial, viral, and parasitic infections in childhood, and how less exposure to these pathogens which leads to allergic diseases in adults. A related hypothesis is that of microbial dysbiosis in which changes in the composition and diversity of microbial communities associated with Western lifestyles somehow contribute to the development eosinophilic esophagitis.
It has also been suggested that environmental factors such as genetic modification or chemical treatment of crops, hormone and antibiotic treatments for livestock, changes in food additives and in processing and food packaging as well as air and water pollutants can contribute to the development of eosinophilic esophagitis.
The reduced frequency of Helicobacter pylori infection may contribute to the increased frequency in eosinophilic esophagitis because data suggest that H. pylori induces T-regulatory cells that protect against allergy development. Alternatively, H. pylori infection may just be a marker of poor hygiene that may protect against allergic diseases, as the hygiene hypothesis suggests. The increased frequency of gastroesophageal reflux disease (GERD) may increase esophageal permeability allowing food allergens to enter the esophageal epithelium leading to eosinophilic esophagitis. acid . The most intriguing hypothesis, however, concerns the use of acid-suppressing drugs.
5. Acid-responsive esophageal eosinophilia is part of a continuum of eosinophilic esophagitis and is not a separate entity
In 2017, guidelines published by a group of European experts including doctors and researchers with expertise in eosinophilic esophagitis officially introduced the concept that Leukocytosis Acid-responsive esophageal eosinophilia is part of a continuum of eosinophilic esophagitis and is not a separate entity. Furthermore, they suggest that anti-acid therapy should be used as first-line therapy and not as a diagnostic test. Most recently, progress from the International AGREE Conference involving US physicians and researchers with expertise in eosinophilic esophagitis also concluded that anti-acids should be classified as First-line treatment for eosinophilic esophagitis is not the diagnostic criterion. 7
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3-20.e6; quiz 21-2. Dellon ES, Jensen ET, Martin CF, et al. Prevalence of eosinophilic esophagitis in the United States. Clin Gastroenterol Hepatol. 2014;12:589-96.e1. Jensen ET, Kappelman MD, Martin CF, et al. Health-care utilization, costs, and the burden of disease related to eosinophilic esophagitis in the United States. AmJ Gastroenterol. 2015;110:626-32. Schoepfer AM, Safroneeva E, Bussmann C, et al. Delay in diagnosis of eosinophilic esophagitis increased risk for stricture formation in a time-dependent manner. Gastroenterology. 2013;145:1230-6.e1-2 Rhonda F. Souza, Eosinophilic Esophagitis: When to Suspect and Why to Treat with Proton Pump Inhibitors, Dispatches from the guild conference, series
19, practicalgastro.