This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
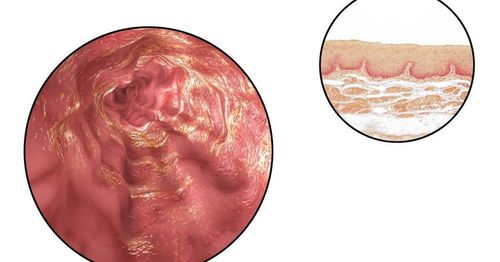
Eosinophilic esophagitis (eosinophilic esophagitis) is a chronic, immune-mediated disease caused by food allergens, presenting with symptoms of dysfunction oesophagitis and esophagitis predominated by eosinophils. Recent consensus guidelines now include proton pump inhibitor therapy as an alternative first-line treatment. This review will discuss why proton pump inhibitors are currently being used as a first-line treatment strategy.
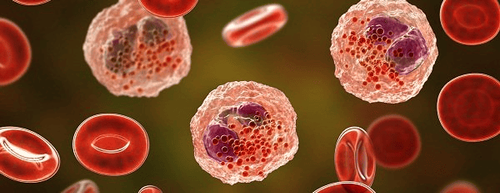
1. Pathogenesis of eosinophilic esophagitis
There is substantial evidence that eosinophilic esophagitis is an allergic disorder. Most patients will present with a food or allergen sensitization on formal allergy testing. In fact, 15% of patients with eosinophilic esophagitis develop food-borne anaphylaxis, a very good reason for referral to an allergist early in the care of these patients.
2. Why do doctors use proton pump inhibitors to treat eosinophilic esophagitis?
It seems paradoxical that antacids are used to treat eosinophilic esophagitis following previous multi-author discussion of how antacids might cause the disease. So let's look at why antacids are used for treatment.
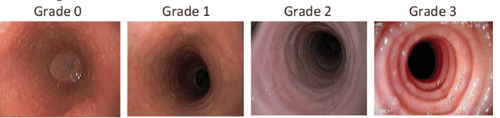
Esophageal symptoms, endoscopic findings, and esophageal eosinophilia are not specific for eosinophilic esophagitis as these features may also be seen in other esophageal conditions including including GERD. Initially, the anti-acid test was used as a diagnostic test for eosinophilic esophagitis because it was assumed that a symptomatic response to an anti-acid meant that the patient had GERD because of the absence of acid secretion. Is there any way that an antigenic condition such as eosinophilic esophagitis might respond to anti-acid drugs?
3. New approaches in eosinophilic esophagitis
In 2007, the if above approach seemed reasonable until investigators began to recognize patients with esophageal symptoms and histology typical of eosinophilic esophagitis, but did not. have evidence of GERD by endoscopy or pH monitoring, and however, those who have responded to antacids. However, at that time, the authors' common definition of eosinophilic esophagitis excluded patients who responded to anti-acids, so investigators had to use a another term to describe such patients and coined the phrase “antacid-responsive esophageal eosinophilia" (anti-acid secretion -REE). Since then, several studies have found a histological response rate of 30% to 50% in patients with esophageal eosinophils treated with antacids.
4. “Esosinophils in the esophagus respond to anti-acid secretion” – A disease separate from eosinophilic esophagitis
In 2011, an interdisciplinary expert panel of eosinophilic esophagitis investigators was convened to update the 2007 consensus recommendations. These updated recommendations removed the requirement. “lack of anti-acid response” from the diagnostic criteria and treat acid-responsive esophageal eosinophilia as a separate and distinct entity from eosinophilic esophagitis. Around the same time, data emerged on the potential anti-inflammatory effects of antacids completely independent of their effect on gastric acid secretion.
5. Basic molecular mechanism of esophageal eosinophilia in response to anti-acids
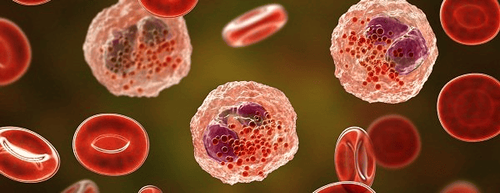
Indeed, Cheng et al. reported that antacids block eotaxin-3 secretion by esophageal epithelial cells that mimic Th2 cytokines in culture. Since these studies were performed on esophageal squamous cells during culture, the anti-inflammatory effect of anti-acids is clearly independent of the effect on gastric acid secretion. Subsequently, Zhang et al showed that antacids induce chromatin remodeling in the eotaxin-3 promoter, resulting in reduced eotaxin-3 transcriptional activity in Th2 cytokine-stimulated esophageal squamous cells culture. Thus, these studies have provided an underlying molecular mechanism of anti-acid-responsive esophageal eosinophilia.
6. Eosinophilic esophagitis unresponsive to antacids is difficult to distinguish from esophageal eosinophilia that responds to antacids.
Multiple clinical studies have shown that eosinophilic esophagitis unresponsive to antacids is indistinguishable from esophageal eosinophilia that responds to antacids based on any clinical findings. , endoscopy or histology showed they were the same disorder. Indeed, studies using RNA microchips have found a similar esophageal transcriptome in patients with eosinophilic esophagitis and acid-responsive esophageal eosinophilia.
Finally, two reports describe patients with eosinophilic esophagitis treated with diet or topical steroids, who for various reasons did not wish to continue those treatments, who are also in remission with anti-acid therapy. In 2017, guidelines published by European experts including physicians and researchers with expertise in eosinophilic esophagitis officially introduced the concept that true eosinophilia antacid response management is part of a continuum of eosinophilic esophagitis and is not a separate entity. Furthermore, they suggest that antacid therapy should be used as first-line therapy rather than as a diagnostic test.
Most recently, progress from the International AGREE Conference involving American physicians and researchers with expertise in eosinophilic esophagitis also concluded that antacids should be classified as First line treatment for eosinophilic esophagitis is not a diagnostic criterion.
7. Management practice considers the use of proton pump inhibitors in eosinophilic esophagitis
It should be noted that the U.S. Food and Drug Administration has to date not approved any drugs for the treatment of eosinophilic esophagitis and all drugs including antihistamines. Acid secretions are used off-label. At multiple large centers, for a patient with esophageal symptoms and an esophageal biopsy showing more than 15 eosinophils/microscopic field, the authors first ruled out non-inflammatory disorders. Eosinophilic esophagitis may induce esophageal eosinophilia (i.e., vasculitis, eosinophilic gastroenteritis, Crohn's disease, and connective tissue disease), to establish the diagnosis of esophagitis. eosinophilia.
Although most gastroenterologists are aware of acid-responsive esophageal eosinophilia, they have been informed for more than 10 years that this condition is not leukoesophageal esophagitis. eosinophils , and it will be some time before the community of practice accepts the view that esophageal eosinophilia in response to antisecretory agents is really just eosinophilic to antisecretory esophagitis. acid . Therefore, after the diagnosis of eosinophilic esophagitis, the authors often start treatment with anti-acid drugs because of its safety, ease of use, and high response rate.

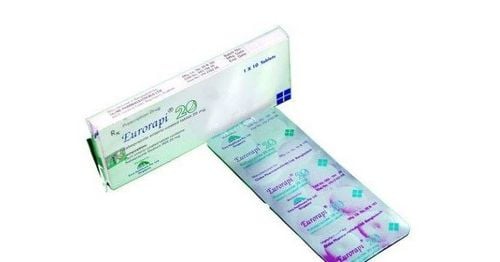
8. How are antacids used in eosinophilic esophagitis?
Antacids were administered twice a day for 4-8 weeks and the authors performed follow-up endoscopy with biopsies while the patient was on antacids to document histological remission. esophageal eosinophils. If the patient responds to antacids, the antacids should be continued.
In a retrospective study, 75 anti-acid-responsive esophageal eosinophilia patients from a European and US cohort were in remission with anti-acids administered more than once per day. days, reduced their antacid dose to once daily with a follow-up endoscopy performed 1 year later. Fifty-five patients (73%) had less than 15 eosinophils/microscopic field and the disease was in remission at 1 year. Another 9 patients (45%) achieved tissue remission when their antacid dose was increased to 40 mg omeprazole twice daily. Thus, it appears that antacid therapy is long-acting to maintain remission in most adults with esophageal eosinophilia who respond to antacids. For patients who do not respond to antacids, a choice is then offered between topical steroids or dietary therapy.
9. Conclusion
Eosinophilic esophagitis is a chronic, antigen-mediated esophageal disorder, the incidence of which has increased dramatically since the early 1990s for reasons that remain unclear. Eosinophilic esophagitis should be suspected in patients with symptoms of esophageal dysfunction, 15 eosinophils/microscopic field on esophageal biopsy, and no abnormalities other than Eosinophilic esophagitis can cause esophageal eosinophilia.
Eosinophils in the esophagus in response to anti-acid secretagogues is known as acid-responsive esophageal eosinophilia, a term that originally emerged from the need to distinguish eosinophilic esophagitis eosinophils with GERD. Since 2007, extensive evidence has supported the view that acid-responsive esophageal eosinophilia lies on the spectrum of an eosinophilic esophagitis continuum rather than a separate entity. separate, separate. Although the term acid-responsive esophageal eosinophilia is still used, it is now a description of eosinophilic esophagitis and not a separate diagnosis. In vitro studies have provided plausible molecular mechanisms for how eosinophilic esophagitis may respond to antiacid therapy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3-20.e6; quiz 21-2. Dellon ES, Jensen ET, Martin CF, et al. Prevalence of eosinophilic esophagitis in the United States. Clin Gastroenterol Hepatol. 2014;12:589-96.e1. Jensen ET, Kappelman MD, Martin CF, et al. Health-care utilization, costs, and the burden of disease related to eosinophilic esophagitis in the United States. AmJ Gastroenterol. 2015;110:626-32. Schoepfer AM, Safroneeva E, Bussmann C, et al. Delay in diagnosis of eosinophilic esophagitis increased risk for stricture formation in a time-dependent manner. Gastroenterology. 2013;145:1230-6.e1-2 Rhonda F. Souza, Eosinophilic Esophagitis: When to Suspect and Why to Treat with Proton Pump Inhibitors, Dispatches from the guild conference, series
19, practicalgastro.