This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
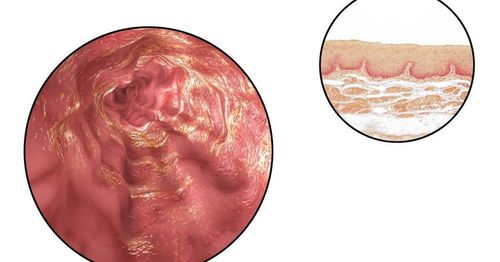
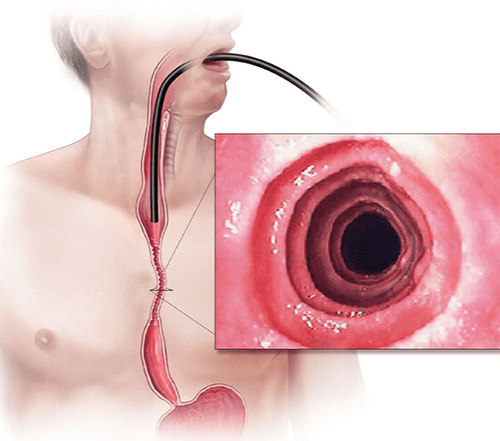
Eosinophilic esophagitis (EoE) is a chronic, immunological or antigenic esophageal disorder that is clinically characterized by symptoms of esophageal dysfunction and histologically by eosinophil infiltration in the esophageal epithelium.
1. The role of genetic susceptibility factors
These data suggest that the pathogenesis of eosinophilic esophagitis begins in a genetically susceptible individual, to whom certain food allergens trigger the immune system. by binding to antigen-presenting cells, which in humans are genetically susceptible, induce a Th2 response to Th2 production of cytokines such as IL-5, IL-4 and IL-13. IL-5 activates eosinophils residing in the bone marrow while IL-13 and IL-4 stimulate the production of eotaxin-3 by esophageal epithelial cells. Eotaxin-3 is a potent chemotherapeutic agent that induces activated eosinophils to reach the esophagus and eosinophils to cause epithelial damage by their degradation products. (Figure 1) Thus, this is a plausible model for the pathogenesis of eosinophilic esophagitis.
2. Proposed hypothesis to explain the increased frequency of eosinophilic esophagitis
Eosinophilic esophagitis was not even recognized until the early 1990s, and its incidence has increased dramatically since then. So why didn't we see eosinophilic esophagitis before 1990, and why are we seeing more now?
The hygiene hypothesis suggests that modern sanitary conditions lead to fewer bacterial, viral and parasitic infections in childhood, and how less exposure to these pathogens which leads to allergic diseases in adults. A related hypothesis is that of microbial dysbiosis in which changes in the composition and diversity of microbial communities associated with Western lifestyles somehow contribute to the development eosinophilic esophagitis.
3. Environmental factors may contribute to the development of eosinophilic esophagitis
It has also been suggested that environmental factors such as genetic modification or chemical treatment of crops, hormone and antibiotic treatments for livestock, changes in food additives and in processing and food packaging as well as air and water pollutants can contribute to the development of eosinophilic esophagitis.
The reduced frequency of Helicobacter pylori infection may contribute to the increased frequency in eosinophilic esophagitis because data suggest that H. pylori induces T-regulatory cells that protect against allergy development. Alternatively, H. pylori infection may just be a marker of poor hygiene that may protect against allergic diseases, as the hygiene hypothesis suggests.
4. Gastroesophageal reflux disease and the use of antacids are associated with eosinophilic esophagitis
Increased frequency of gastroesophageal reflux disease (GERD) may increase esophageal permeability allowing food allergens to enter the esophageal epithelium resulting in leukocytosis esophagitis craving. The most intriguing hypothesis, however, concerns the use of acid-suppressing drugs. pylori infection may just be a sign of poor hygiene that may protect against allergic diseases, as the hygiene hypothesis suggests. The increased frequency of gastroesophageal reflux disease (GERD) may increase esophageal permeability allowing food allergens to enter the esophageal epithelium leading to eosinophilic esophagitis. acid .
However, the most compelling hypothesis concerns the use of acid-suppressing drugs. pylori infection may just be a sign of poor hygiene that may protect against allergic diseases, as the hygiene hypothesis suggests. The increased frequency of gastroesophageal reflux disease (GERD) may increase esophageal permeability allowing food allergens to enter the esophageal epithelium leading to eosinophilic esophagitis. acid . The most intriguing hypothesis, however, concerns the use of acid-suppressing drugs.
5. Anti-acid drugs have been found to increase the permeability of the gastric mucosa
The dramatic increase in the frequency of eosinophilic esophagitis began in the early 1990s, just as the therapeutic use of antacids became widespread. As we discussed earlier, on a daily basis, we ingest a large number of protein allergens that are capable of generating an immune response. When a protein allergen enters the stomach, it is digested by pepsin into small peptides that may no longer cause an allergic reaction.
However, antacids increase gastric pH to levels above 4.5, at which pH the enzymatic activity of pepsin is no longer active. In addition, antacids were found to increase the permeability of gastric mucosa. Thus, allergenic peptides are not broken down in the stomach, and are instead absorbed intact through the gastric mucosa or through the small intestine, where they can cause an allergic reaction. Interestingly, there is some empirical support for this hypothesis. Food-specific IgE antibodies may develop in patients taking antacids or H2-receptor blockers for three months, despite a negative history for allergies or allergies. However, after three months of acid-reducing therapy, 10% of patients had an increase in their available IgE levels and 15% of patients without detectable IgE at baseline developed new IgE antibodies. , which is specific to food suggests that acid-suppressing drugs can lead to the development of food allergies.

6. The association between prenatal, intrapartum and postpartum factors and the risk of developing eosinophilic esophagitis
Furthermore, a recent case-control study explored the association between prenatal, intrapartum, and postpartum factors and the risk of developing eosinophilic esophagitis later in childhood. . Several prenatal factors are significantly associated with eosinophilic esophagitis including maternal fever, pregnancy complications, and preterm labor. Caesarean section is also associated with later development of eosinophilic esophagitis. Postpartum, in the neonatal period, antibiotic use has been associated with eosinophilic esophagitis while keeping a dog or cat at home is a protective measure. However, the strongest risk factor for the development of eosinophilic esophagitis later in childhood is the use of acid-suppressing drugs during the first year of life.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3-20.e6; quiz 21-2. Dellon ES, Jensen ET, Martin CF, et al. Prevalence of eosinophilic esophagitis in the United States. Clin Gastroenterol Hepatol. 2014;12:589-96.e1. Rhonda F. Souza, Eosinophilic Esophagitis: When to Suspect and Why to Treat with Proton Pump Inhibitors, Dispatches from the guild conference, series
19, practicalgastro.