This is an automatically translated article.
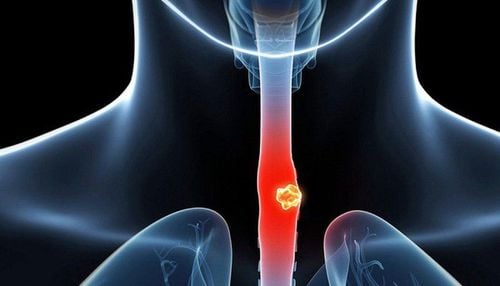
The article is written by MSc, BS. Mai Vien Phuong, Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalThe application of artificial intelligence in early diagnosis of esophageal cancer actively supports the treatment of this dangerous cancer. The following article will help you better understand artificial intelligence and its application in the diagnosis of Barrett's esophagus and esophageal cancer.
1. Overview of artificial intelligence
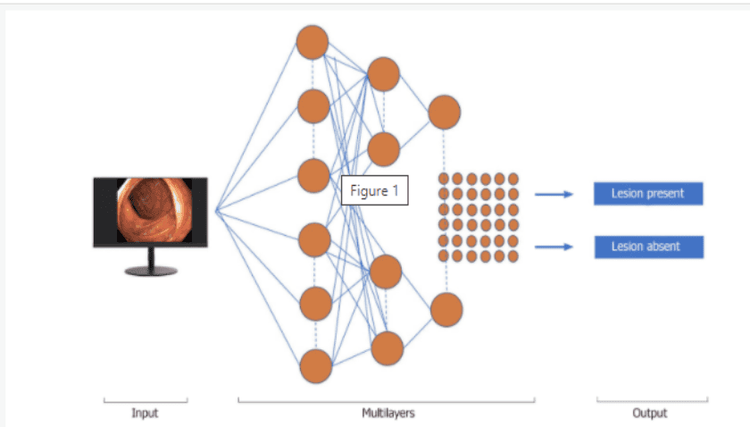
Artificial intelligence (AI) is based on artificial intelligence elements that perform functions related to the human mind, such as learning and problem solving.In colonoscopy, AI has begun to aid in improving colon polyp detection and adenoma detection (ADR) rates, to distinguish between benign and precancerous lesions based on the interpretation of patterns their surface.
Machine learning (ML) and deep learning (DL) can be considered as subfields of artificial intelligence. ML is a form of artificial intelligence that can support decision-making, allowing improvements to applied algorithms without programming, including examining data and implementing descriptive models and models. predicted (Figure 1).
2. What is Barrett's esophagus?
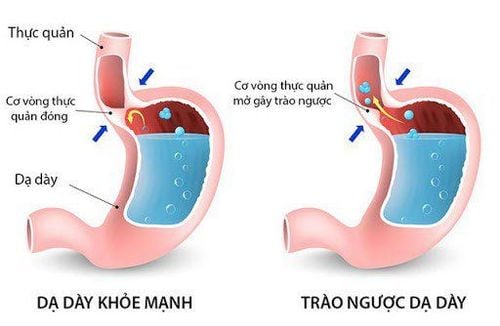
Barrett's esophagus (BE) is characterized by abnormal transformation (hyperplasia) of the cells of the mucosa, lining the lower part of the esophagus, from normally stratified squamous epithelium to columnar and associated epithelium. alternate cup-shaped cells. This condition represents a risk factor for esophageal adenocarcinoma (EAC) whose most severe prognosis is related to late diagnosis. Furthermore, 93% of patients can achieve complete remission after regular treatment and follow-up for 10 years. Promising techniques for the management of Barrett's esophagus, with the potential to reduce cancer risk by accurately diagnosing dysplasia, are under development.3. The role of endoscopic diagnosis of Barrett's esophagus
However, despite some limitations in interventional therapies, such as endoscopic mucosal resection (EMR) and radiofrequency ablation or cryotherapy, they can help prevent prevent progression to malignancy.It is important to document neoplastic changes in patients with Barrett's esophagus, and changes in endoscopic images have helped in the early detection of minimal neoplastic lesions based on individual features. mucosal differentiation.
4. Artificial Intelligence, Barrett's Esophagus and Esophageal Cancer
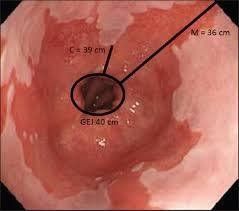
In the first study, Mendel et al., introduced a useful method to generate automatic classification based on endoscopic white light images by learning specific features supported by the network. Digitized data is processed from multiple source codes, rather than manually processed features. The study used a dataset of 100 high-resolution endoscopic images from 39 patients provided by the Computer Aided Intervention and Endoscopic Imaging (MICCAI) system. While 22 patients with Barrett's esophagus had cancerous lesions, 17 patients with Barrett's esophagus were not cancerous.The endoscopic images were independently evaluated by five experts and then compared with the AI-powered probability map, showing strong correspondence. As the importance of manual segments differed significantly, their intersection was considered as the cancer region (C1 region) in each C1 image.
5. Some studies of AI in esophageal cancer diagnosis
Ebigbo et al., used two datasets to train and validate a computer-aided diagnostics (CAD) system based on a CNN computer network with residual network (ResNet) architecture. Imaging includes 148 high-definition white light endoscopic (WLE) and narrowband imaging (NBI) images involving 33 esophageal cancer regions and 41 noncancerous Barrett esophagus regions in the Augsburg dataset , while the MICCAI dataset includes 100 high-definition WLE images, 17 early EACs, and 22 noncancerous Barrett esophagus fields. The CAD-DL system diagnosed EAC with 97% sensitivity and 88% specificity for WLE images, while sensitivity and specificity were 94% and 80% for NBI images, respectively. The CAD-DL system achieved sensitivity and specificity of 92% and 100% for MICCAI imaging, respectively.In these early studies, the authors developed a CAD computer model and displayed promising performance scores in the classification/segmentation domains during the assessment of Barrett's esophagus.
However, these results are achieved using high-quality endoscopic images that are not always obtained during daily clinical practice. This system was previously developed to further speed up image analysis for classification and resolution of dense predictions, displaying the color-coded spatial distribution of cancer probabilities.
6. The role of Complex Neural Networks CNN in artificial intelligence
Still based on the complex neural network system CNN and ResNet architecture with DeepLab V.3+, a modern reconfigured encoder-decoder network. To transmit the endoscope Livestream to our AI system, a capture card (Avermedia, Taiwan) for image transmission was integrated into the endoscope screen and the AI system was trained using 129 images. Endoscopic. All AI imaging findings were confirmed by pathological examination of resected samples of esophageal cancer as well as clamp biopsies (ie, Barrett's esophagus alone). The AI system showed a high performance score in lesion classification with sensitivity and specificity of 83.7% and 100%, respectively.
7. The role of the HD-WLE system and the NBI . system
AI can assist endoscopists to do targeted biopsies with high accuracy, save work/time-consuming random sampling, with low sensitivity (64%) for detecting metaplasia. An international, randomized, crossover trial comparing high-definition white light endoscopy (HD-WLE) and NBI for the detection of IM and malignancy in 123 patients with BE (mean circumference and maximum size, 1.8 and 3.6 cm, respectively).Both the HD-WLE system and the NBI system detected 104/113 (92%) patients with intestinal metaplasia, but the NBI required fewer biopsies per patient and showed a higher detection rate of dysplasia significantly (30% vs. 21%). During endoscopic examination with NBI, all areas of high-grade dysplasia and cancer showed mucosal or vascular irregularities. Surface samples observed with the conventional NBI system did not contain high-grade dysplastic or cancerous lesions, suggesting that biopsy could be avoided in the following cases.
8. Using endoscopic trimodal imaging (ETMI) to detect early cancer in Barrett's esophagus
In a randomized, multicenter, crossover study using endoscopic trimodal imaging (ETMI) for early cancer detection in Barrett's esophagus, ETMI did not show an improvement in the overall detection of dysplasia compared with with standard video endoscopes. The diagnosis of dysplasia is still made in a substantial number of patients by random biopsy, and patients with a confirmed diagnosis of low-grade LGIN intraepithelial neoplasia have a significant risk of neoplasia. HGIN high-grade epithelial/carcinoma.Van der Sommen et al used a computer algorithm to detect early cancerous lesions in Barrett's esophagus and used specific textures, color filters and based machine learning algorithms based on 100 images Photos from 44 patients with Barrett's esophagus. This system identifies early cancer lesions at the patient level with sensitivity and specificity of 86% and 87%, respectively. The author assumes that the automated computer algorithm implemented for this study can identify early cancerous lesions with reasonable accuracy.
De Groof et al developed a CAD system using endoscopic images of Barrett cancer based on endoscopic images of 40 Barrett cancerous lesions and 20 Barrett's esophagus without dysplasia, achieving sensitivity and The specificity for detecting such lesions is 95% and 85%, respectively.
9. Volumetric laser endoscopy (VLE) technology in esophageal cancer diagnosis
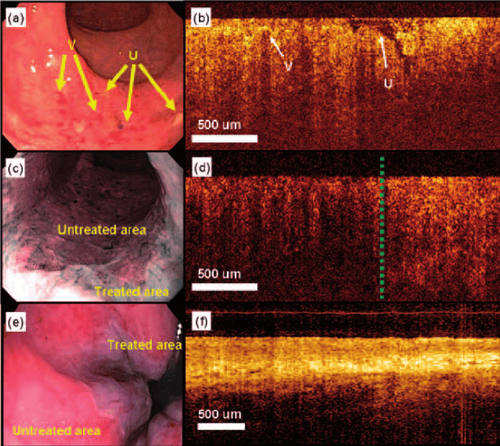
AI technology was applied to volumetric laser endoscopy (VLE) in 2017. VLE with laser marking is a broad field of advanced imaging technology that was commercialized in the United States in 2017. 2013 to facilitate the detection of dysplasia.VLE can enhance detection of neoplastic lesions in Barrett's esophagus by performing circumferential scanning of the esophageal wall layers. Sixteen patients with Barrett's esophagus were included in the study and a total of 222 laser markers (LMs) were placed, 97% of them visible on WLE. All LMs were clearly visible on the VLE immediately after marking, and 86% were confirmed during post-school analysis. Laser targeting LM has 85% accuracy of traces. This initial study applied to humans suggests that VLE-guided LM may be a viable and safe procedure.
In another study, the same author used a database of VLE images from Barrett's esophagus with/without tumor, accurately correlating them with histology to develop scores VLE prediction. The receiving performance curve of this predictor shows an area under the curve (AUC) of 0.81. A value of ≥ 8 correlates with a sensitivity of 83% and a specificity of 71%.
10. The role of optical tomography (OCT) in the diagnosis of esophageal cancer
Optical tomography (OCT) is a technique that creates high-resolution images of the esophagus through an endoscope. OCT can identify specific intestinal metaplasia from epithelial squamous cells, but imaging criteria to distinguish intramucosal carcinoma (IMC) and low-grade dysplasia from high-grade dysplasia, acute dysplasia Grade indeterminate (IGD) and specific bowel metaplasia without dysplasia have not yet been approved.Evans et al., examined 177 OCT images from patients with the histological diagnosis of Barrett's esophagus. Histopathological analysis was IMC/HGD in 49 cases, LGD in 15, IGD in 8, specific IM in 100, while gastric mucosa in 5 patients. A significant correlation was found between the histopathology of mucosal cancer or high-grade dysplasia and the scores for each of the imaging features, extent of surface abnormalities, and glandular architecture. When using a dysplasia index ≥ 2 determination, 83% sensitivity and 75% specificity were determined for the diagnosis of IMC/HGD.
In a community health care center, 27 Barrett's esophagus patients who underwent 50 EMR mucosalectomy procedures were imaged with VLE and pCLE, and classified as cancerous/non-cancerous in the body histological results. The sensitivity and specificity of pCLE for the detection of Barrett's esophagus were 76% and 79%, respectively. OCT-SI showed a sensitivity of 70% and specificity of 60%. Furthermore, the VLE-DA technique showed a sensitivity of 86%, a specificity of 88% and a diagnostic accuracy of 87%.
Esophageal squamous cell carcinoma (SCC) is the sixth leading cause of death worldwide and a greater percentage affects developing countries due to delayed diagnosis. Esophageal endoscopy using Lugol dye is currently the gold standard technique to identify SCC during gastroscopy, although the specificity is low (about 70%) but the sensitivity is higher (over 90%).
11. Microscopic endoscopy (magnification at the cellular level) and esophageal cancer
High-resolution microscopic (at the cellular level) endoscopy (HRME) has shown the potential to enhance the detection of esophageal SCC during screening. An automated, real-time analysis algorithm was developed and evaluated using training and validation tests obtained from a previous in-vivo study involving 177 subjects. for screening/surveillance programs. In a post-analysis, the algorithm recognized malignancies with 95% sensitivity and 91% specificity, in the validation dataset, compared with 84% and 95% in the original study. The technology could therefore be applied in facilities where operators have less expertise in interpreting HRME images.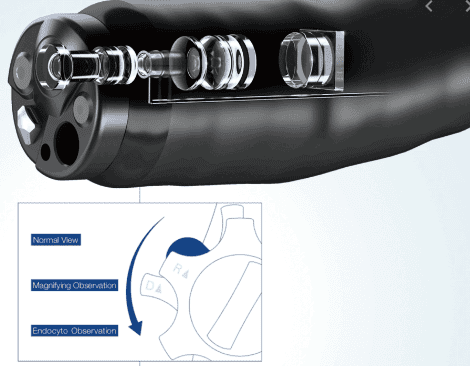
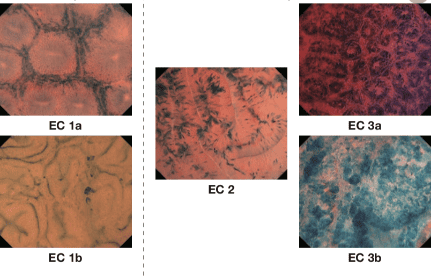
12. Assessment of invasiveness of esophageal cancer lesions by AI
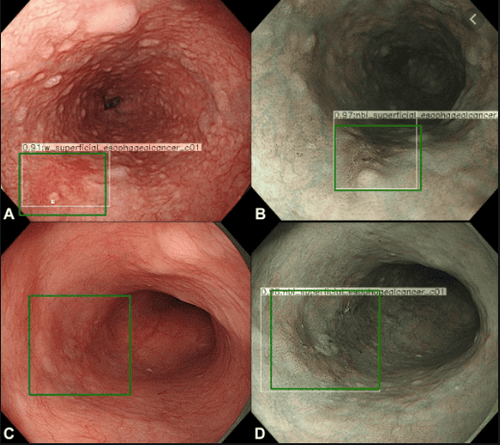
The highest performance was obtained using the mean nuclear region as input for classification, resulting in a sensitivity and specificity of 93% and 92% in the training set, and 87% and 97% in the test set. , 84% and 95% in the set of independent validators, respectively. EMR mucosal resection is a technique used to treat tumors with submucosal depth of invasion 1 (SM1), while surgical resection with/without chemotherapy is commonly used for cases of SCC with tumor infiltrating deeper than SM2.Accordingly, preoperative endoscopic estimation of the depth of invasion of ESCC is important. Recently, a rapid improvement in the application of AI with DL in medicine has been realized. A study by Tokai et al., evaluated the effectiveness of AI in measuring the depth of invasion of ESCC in a set of 1751 ESCC training images. The AI recognized 95.5% (279/291) of ESCC in 10 test images when analyzing 279 images it accurately predicted ESCC depth of invasion with 84.1% sensitivity and accuracy 80.9% in 6 s, much more accurate for ESCC estimates of depth of invasion from endoscopists.
To actively protect health, subjects over 40 years old with a history of atrophic gastritis, chronic gastritis; Barrett's esophagus; submucosal tumors need periodic examination; People with anemia of unknown cause, after gastrectomy, family history of stomach cancer should be screened for gastrointestinal cancer periodically. Currently, Vinmec offers a package of screening and early detection of cancers of the gastrointestinal tract (esophagus - stomach - colon) combining clinical and paraclinical examination to bring about the most accurate results possible. With this package, you will get:
Gastroenterology Specialist Examination; Gastroscopy and colonoscopy with NBI endoscope under anesthesia; Gastroscopy and colonoscopy with anesthesia; Routine histopathological examination of fixation, transfer, casting, cutting, staining... of biopsies (upper gastrointestinal tract (esophagus, stomach, duodenum, papilla) through endoscopic examination; Histopathological examination Routinely fix, transfer, cast, cut, dye... biopsies (lower gastrointestinal tract through endoscopy (colon, rectum). Vinmec, please register to book an appointment right at the website or contact Vinmec's hotline for detailed advice.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesRussell S, Norvig P. Artificial Intelligence: A Modern Approach, Global Edition. 3rd editon. London: Pearson, 2016. Gaetano Cristian Morreale, Emanuele Sinagra, et al., Emerging artificial intelligence applications in gastroenterology: A review of the literature , Artif Intell Gastrointest Endosc. Jul 28, 2020; 1(1): 6-18