This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalDue to the rapid progression and poor prognosis of esophageal cancer (EC), the early detection and diagnosis of esophageal cancer is of great value in improving the prognosis for patients. Currently, science has applied artificial intelligence in endoscopic methods to diagnose early esophageal cancer.
Abbreviation:
EC: Esophageal cancer
AI: artificial intelligence
BE: Barrett esophagus
1. What is Artificial Intelligence?
Artificial Intelligence (AI: Artificial Intelligence) can be defined as a branch of computer science that deals with the automation of intelligent behaviors. AI is a part of computer science, and therefore it must be based on sound, applicable theoretical principles of the field.

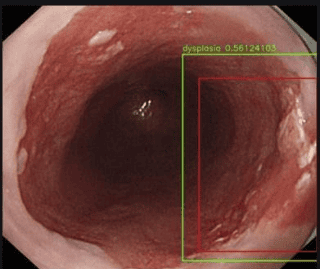
2. Overview of the application of artificial intelligence to gastrointestinal endoscopy
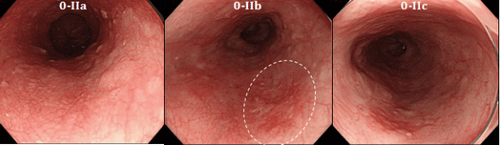
Due to the rapid progression and poor prognosis of esophageal cancer (EC), the early detection and diagnosis of esophageal cancer is of great value in improving the prognosis for patients. However, early endoscopic detection of esophageal cancer, especially Barrett dysplasia or esophageal squamous dysplasia, is difficult. Therefore, the demand for more effective methods of detecting early esophageal cancer features has led to intensive research in the field of artificial intelligence (AI). Deep learning and memory techniques (DL) have brought breakthroughs in image, video and other aspects of processing, while complex neural networks (CNN) have paved the way for detect high-resolution endoscopic images and videos.
3. Introduction to esophageal cancer
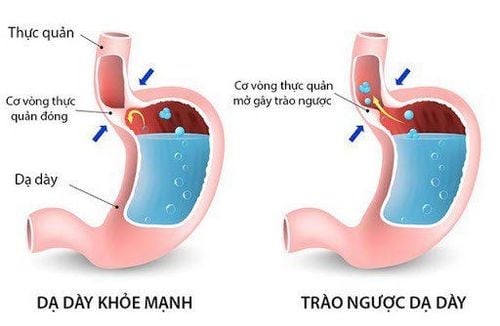
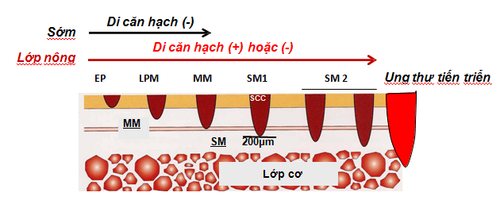
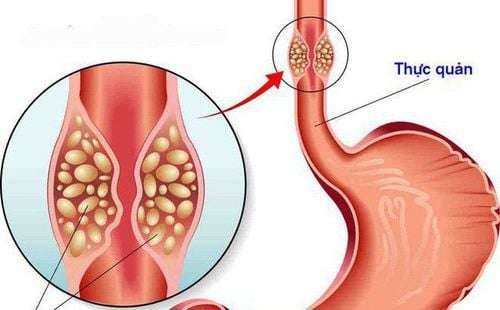
Esophageal cancer (EC) is the eighth most common cancer and the sixth leading cause of cancer death worldwide. Esophageal cancers mainly include esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC). Esophageal adenocarcinoma is the most common disease in Western countries, more than 40% of patients with esophageal adenocarcinoma are diagnosed after the disease has metastasized and the 5-year survival rate is less than 20. %.
Although the incidence of esophageal adenocarcinoma is increasing globally, esophageal squamous cell carcinoma remains the most common (80%) of all esophageal cancers with the highest incidence on the "cancer belt" extending from East Africa and through the Middle East to Asia. Only 20% of patients with esophageal squamous cell carcinoma survive longer than 3 years, mainly due to late-stage diagnosis. In low-resource areas, the 5-year survival rate is much lower at around 3.4%. Early diagnosis can significantly improve outcomes for all esophageal cancers.
4. The role of artificial intelligence AI in early detection of esophageal cancer
4.1. Barrett's dysplasia and early esophageal adenocarcinoma
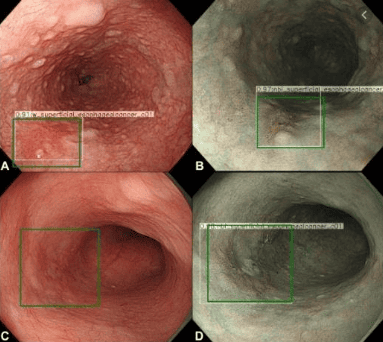
Artificial intelligence AI based on white light endoscopy (WLE) and NBI narrowband endoscopy system : There are some limitations to recognize early cancerous lesions associated with Barrett's esophagus by WLE, a common technology. High-definition WLE (HD-WLE) and NBI endoscopy systems were once considered to improve the accuracy of the diagnosis of early cancerous lesions associated with Barrett's esophagus. But the improvement has yet to satisfy endoscopists. This situation stimulated the development of a CAD system for early cancerous lesions in Barrett's esophagus based on a supervised ML blood learning algorithm. However, this system still has difficulty in identifying early cancerous lesions associated with Barrett's esophagus and selecting biopsy sites. The accuracy of the system using HD-WLE is better than that of the general endoscope system. Moreover, the system shows the ability to locate the lesions and the regional matching rate between the lesions by the system and local experts is up to 72%. In general, the specificity of NBI is higher than that of conventional WLE. Compared to using HD-WLE, the system has no obvious advantage when using NBI system.
5. Role of endoscopic coherence optical tomography (EOCT) and endoscopic confocal laser (CLE)
AI artificial intelligence based on endoscopic optical tomography and confocal laser: In addition to WLE and NBI, endoscopic optical coherence tomography (EOCT) and endoscopic laser confocal ( CLE) is also used for early diagnosis of EAC/BE-associated dysplasia. EOCT can identify early tumor lesions associated with Barrett's esophagus by analyzing mucosal and submucosal structures of the esophagus. CLE can observe mucosal tissue and cell morphology to achieve optical biopsies. However, the complexity of these two imaging technologies, the time-consuming reading of the images, and the requirement of a senior endoscopist have limited their clinical use. To solve this problem, Qi et al extracted multiple EOCT imaging features and combined one or more features to classify lesions, but the results were not satisfactory. Then, Swager et al used volumetric laser endoscopic imaging (VLE, integrated with second-generation OCT) for training and testing, and the results showed that the CAD system was superior to VLE experts. Veronese et al used CLE imaging, and the results showed that the system was able to accurately differentiate gastric (GM), intestinal (IM) and neoplasia. Ghatwary et al. showed that the sensitivity of the system using CLE imaging to diagnose IM and cancer was significantly higher than that of the system for diagnosing GM. Similarly, the CAD system established by Hong did not identify the GM, the diagnostic sensitivity of IM was not significantly different from the above study, and the sensitivity for cancer diagnosis was also slightly reduced. This may be due to the limited number of GM and neoplastic images. Currently, there is little clinical research in this area and the available images are limited. In the future, more studies are needed to confirm the value of VLE/CLE combined with AI in early diagnosis of EAC.
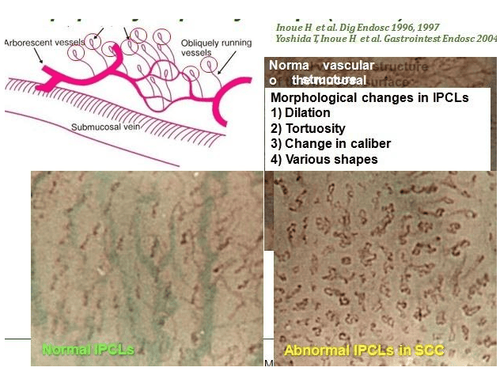
6. The role of artificial intelligence AI in endoscopy (endoscopy at the cellular level)
AI artificial intelligence based on high resolution endoscopy and microscopic endoscopy: Endoscopic endoscopy (endoscopy at the cellular level) is a new technology that combines magnifying endoscopy with important dye. Due to the excellent magnification, the endoscope can clearly visualize the epithelial cells of the esophageal mucosa to achieve an effect similar to the diagnosis of pathology. However, if endoscopists want to use endoscopy to independently complete real-time detection, they need a strong background in pathology, which is clearly impractical. Therefore, AI may be the best choice to aid in endoscopic diagnosis. Kumagai et al. have shown that the performance of the system using higher magnification images is better than the system using lower magnification images. However, no stratified analysis of superficial and advanced esophageal cancer was included in this study. The results may not accurately reflect the ability of endoscopy combined with AI to diagnose early esophageal cancer. High-resolution microscopy (HRME) can be used to observe esophageal mucosal tissue and cell morphology. Shin et al tested the ability of different imaging features to differentiate tumors from non-tumor lesions, and the best features were selected with 84% sensitivity and 95% specificity. . However, it takes a long time to analyze an image and the sensitivity is not ideal. In the future, more high-quality studies are needed to confirm its role in early esophageal cancer diagnosis.
6.1. Real-time endoscopic diagnosis using AI
Quang et al. used the same HRME imaging data as Shin et al for training and validation, the results showed a sensitivity of 95% and specificity of 91% in the early diagnosis of esophageal cancer. Then, three patients with suspected esophageal cancer were examined endoscopically with 100% accuracy. However, there are some limitations in this study.
First, the number of patients and images in real-time diagnosis is too small. Second, the system still uses images for diagnosis, not video for real-time detection. Everson et al and Guo et al established a DL-based CAD system with good diagnostic performance using NBI narrowband video. Unfortunately, these systems have not been applied in real-time diagnostics.
6.2. The role of AI in the histopathological diagnosis of early esophageal cancer
Although AI combined with endoscopic diagnosis has made many advances, endoscopic diagnosis still cannot replace the gold standard in pathology. However, there is a problem in the pathological diagnosis of early esophageal neoplasia, that is, the accuracy of the diagnosis of dysplasia is not ideal with significant variation between the host of observations. To address this issue, Sabo et al established two models to distinguish non-dysplasia (ND) from low-grade dysplasia (LGD) and LGD from high-grade dysplasia (HGD) by image extraction. pathological sections stained with hematoxylin and eosin (HE). Characteristics of patients with Barrett's esophagus BE. The results showed that the two models performed well in the diagnosis of indistinguishable contour lesions. Baak et al combined the HE-stained pathologic cross-sectional imaging features with the immunohistochemical indices p53/Ki67 and used endoscopic gastrointestinal resection specimens and biopsies. Barrett's esophagus for testing. It was found that the system performed well in distinguishing ND from LGD and LGD from HGD. However, the accuracy of distinguishing HGD from intramucosal carcinoma needs to be improved. The performance of the system is better than that of a general pathologist and only slightly worse than that of an experienced pathologist.
6.3. The role of artificial intelligence AI in risk stratification of early esophageal cancer
It is estimated that only 0.12% -0.43% of patients with Barrett's esophagus may progress to early esophageal cancer each year, it is particularly important to establish an effective model to predict the risk of esophageal cancer. of early esophageal cancer each year in patients with Barrett's esophagus. Previously risk stratification was based primarily on the presence of dysplasia, but its efficacy was not ideal. Critchley-Thorne et al established a predictive model based on the characteristic differences in immunofluorescence markers and histopathology, specifically between patients with Barrett's esophagus who developed cancer. early esophagus each year and those without the disease. Results have not been encouraging, with more than 30% of Barrett's esophagus patients developing early esophageal cancer each year being classified as low-risk.
Artificial intelligence AI is trying to be used for endoscopic detection, pathological diagnosis, genetic diagnosis and cancer risk prediction of early esophageal cancer. It is useful for endoscopists and pathologists to improve diagnostic accuracy and assist physicians in treatment and follow-up strategies.
Currently, gastrointestinal cancer screening is a scientific and effective measure for early detection of gastrointestinal cancer (esophageal cancer, stomach cancer, colon cancer) and giving a treatment plan. best treatment. Currently, Vinmec International General Hospital has a package of screening and early detection of cancers of the gastrointestinal tract (esophagus - stomach - colon) combined with clinical and paraclinical examination to bring the most accurate results. maybe.
When screening for gastrointestinal cancer at Vinmec, you will receive:
Gastrointestinal specialty examination with an oncologist (by appointment). Gastroscopy and colonoscopy with an NBI endoscope under anesthesia. Complete peripheral blood cytology (by laser counter). Automated prothrombin time test. Automated thrombin time test. Activated Partial Thromboplastin Time (APTT) test using an automated machine. General abdominal ultrasound
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Bray F , Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin . 2018; 68 :394-424. [PubMed] [DOI] Hur C, Miller M, Kong CY, Dowling EC, Nattinger KJ, Dunn M, Feuer EJ. Trends in esophageal adenocarcinoma incidence and mortality. Cancer . two thousand and thirteen; 119 :1149-1158. [PubMed] [DOI] Thrift AP . The epidemic of oesophageal carcinoma: Where are we now? Cancer Epidemiol. 2016; 41 :88-95. [PubMed] [DOI] Lu-Ming Huang, Wen-Juan Yang, Zhi-Yin Huang, Cheng-Wei Tang, Jing Li, Artificial intelligence technique in detection of early esophageal cancer, World J Gastroenterol. Oct 21, 2020; 26(39): 5959-5969