This is an automatically translated article.
Evolution of procalcitonin levels can be used as a parameter for differential diagnosis and early assessment of sepsis and sepsis. PCT quantification should be performed and monitored daily. For special cases, dosing should be done in short intervals of 8 to 12 hours.
1. Quantification of Procalcitonin
Procalcitonin, or PCT for short, is produced by C cells in the thyroid gland or other cells in the body such as liver cells, lungs, monocytes... when stimulated by a severe injury, especially in infections. systemic bacteria. PCT is made up of 116 amino acids which are precursors of the hormone calcitonin.
Bacterial endotoxins, proinflammatory cytokines, IL-6 and TNF-α are the main derivatives in the mechanism of PCT proliferation, but the liver is still the major site of PCT synthesis and release. The half-life of PCT in plasma ranges from 19-24 hours.
2. Order PCT . test
The Procalcitonin test is a relatively new test but it is gradually becoming more used. Recent studies have demonstrated a role for PCT in assessing the risk of systemic infections in critically ill patients. It is indicated primarily in patients admitted to the emergency department, in intensive care, or in patients with suspected sepsis. Procalcitonin test has been recognized by FDA as an aid in assessing the risk of sepsis and septic shock in critically ill patients. PCT is often quantified in the early days of disease for diagnosis. It may be done later to monitor response to treatment.
Procalcitonin may be done with other tests such as CRP, complete blood count, blood culture, and lumbar puncture to detect or rule out acute infection, to differentiate bacterial meningitis from viral, or to detect and exclude bacterial pneumonia in severe patients and in children with unexplained fever. Procalcitonin is also indicated when there is tissue damage due to causes such as trauma, surgery, or detection of bacterial superinfection in patients with viral pneumonia Procalcitonin is also used to monitor the effectiveness of treatment of the condition. infection.

Xét nghiệm Procalcitonin đã được dùng hỗ trợ đánh giá nguy cơ nhiễm khuẩn huyết, sốc nhiễm khuẩn ở những bệnh nhân nặng
3. Diagnosis of infection
The normal value of human plasma PCT is < 0.046 ng/mL (or < 0.046 μg/L). A clinically significant cut-off value is: < 0.5 ng/mL: low risk for severe infection or septic shock; > 2.0 ng/mL: high risk for severe infection or septic shock.
PCT is a specific parameter of severe bacterial inflammation and fungal infections and is a true indicator of inflammatory activity associated with infection and multiple organ failure. Therefore, the evolution of PCT concentration can be used as a parameter to differentiate acute infection and monitor the degree of inflammation due to infection. PCT quantification should be performed and monitored daily. For special cases, dosing should be done in short intervals of 8 to 12 hours.
Elevated plasma PCT levels in various diseases:
Chronic inflammation, autoimmune disorders, viral infections (eg, HBV infection), mild or local infections: PCT < 0.5 ng/mL Pneumonia : PCT 0.5-10 ng/mL Systemic inflammatory response syndrome, multiple trauma, burns: PCT 0.5-2 ng/mL Severe infection, sepsis, multi-organ failure: PCT > 2 (usually is 10-100 ng/mL). In severe infectious inflammatory diseases and multi-organ dysfunction syndromes, elevated levels of PCT reflect inflammation. The advantage of PCT over other inflammatory markers is that severe infections strongly increase PCT (with levels > 10 ng/mL), whereas mild infections or milder periods of infection only cause moderately increased levels of blood PCT. CRP is maximal in moderate infections. If the trigger goes away, it means that after successful treatment, PCT levels return to normal within a few days. In peritoneal infection, a decrease in PCT level during the first 3 days is a good indicator of survival with a sensitivity of 84% and specificity of 91%. Similarly, in patients with multiple organ failure syndromes or infections, persistent and persistent elevations in PCT levels represent a persistent inflammation and are indeed a poor prognostic marker. In dying patients, PCT levels are persistently elevated.
4. Bacteremia
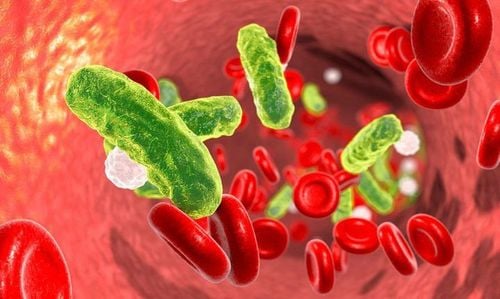
Nhiễm khuẩn huyết xảy ra do vi khuẩn hay virus, nấm giải phóng những hóa chất vào máu
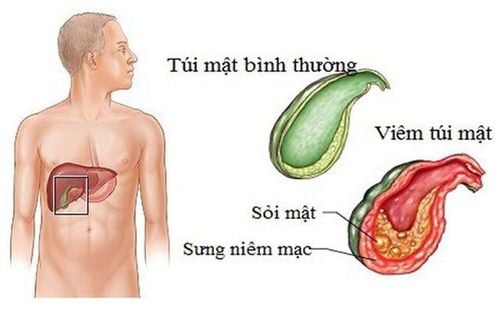
Sepsis is caused by bacteria or viruses, fungi release chemicals into the bloodstream to fight the body's inflammatory response, is a very serious infection. Pathogenic microorganisms do not reside in an initially damaged organ, but spread through the bloodstream throughout the body.
These reactions create a series of internal changes that lead to damage to organs such as: Liver, kidneys, and rapid deterioration of the body. PCT has many advantages over other markers CRP, Interlekin. This is a specific marker for infection and sepsis. It is produced specifically by non-viral infections, is not affected by viral infections or other autoimmune responses, and blood PCT levels are independent of renal function. Low PCT levels have high negative prognostic value to rule out sepsis and conversely, high PCT levels confirm the diagnosis of infection, sepsis, and septic shock, especially when there is dysfunction of the muscles. organs, the consequences of systemic inflammation, multiple organ failure...
In general, patients with suspected bacterial infection or sepsis, patients at special risk (after surgery, immunosuppressive ...) are patients who should be monitored for PCT, and researchers recommend that in cases of suspected sepsis, PCT should be tested immediately, if negative, repeated every 6 hours to capture a response. earliest diagnostic response. To monitor disease progression and effectiveness of treatment, PCT testing should be performed once a day. Infection was controlled if PCT levels decreased by 30-50% by day.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
MORE:
Diagnosing septic shock When does septic shock occur? What is bacteremia?