This is an automatically translated article.
Inotropic agents are the mainstay of treatment for heart failure and cardiogenic shock, are routinely used in ICUs and are considered by physicians for treatment of chronic heart failure. count. Despite the effect of increasing the stroke volume of the heart, many studies have shown that inotropic drugs can increase the risk of death due to increased heart rate, arrhythmia, myocardial ischemia. New generation inotropic drugs have opened up new prospects, helping to increase myocardial contractility, reduce side effects, and prolong patient's life.1. Classic inotropic drugs
1.1. Digoxin
Digoxin belongs to the group of drugs Digitalis has the effect of inhibiting the enzyme Na+-K+-ATPase in the cell membrane, leading to increased myocardial contractility, positive fiber contraction effect. In addition, Digoxin also has a direct reduction in heart rate and heart rate through parasympathetic stimulation, slowing conduction in the atrioventricular node. In patients with symptoms of heart failure, left ventricular ejection fraction <40%, and atrial arrhythmias, use of digoxin may reduce symptoms and risk of hospitalization due to progression of heart failure. Digoxin not only improves hemodynamics in patients at rest but also during exercise. However, according to the 1997 DIG (Digitalis Investigation Group) study, digoxin did not improve mortality from heart failure. Since the publication of DIG, the use of digoxin as an inotropic agent for the treatment of heart failure has decreased significantly. However, the role of Digoxin in heart failure is still very important.
Some points to note when using Digoxin as an inotropic agent are:
Digoxin is eliminated by the kidneys, so the dose should be reduced or avoided in patients with renal impairment. Digoxin is a drug with a narrow therapeutic range, easy to accumulate and cause toxicity. Therefore, if possible, it is necessary to check the concentration of Digoxin in the blood to adjust the dose accordingly. It should be noted that some drugs can interact with Digoxin, increasing the concentration of Digoxin in the blood, causing poisoning such as Amiodarone, Diltiazem, Verapamil, Quinidin, some antibiotics,...

Bệnh nhân suy thận nên cân nhắc khi sử dụng thuốc
1.2. Dobutamine
Dobutamine is a synthetic catecholamine, has the effect of making the heart muscle contract, used in acute heart failure (found in cardiogenic shock, myocardial infarction). Dobutamine is also used in septic shock. For chronic congestive heart failure, dobutamine can be used to treat but must be cautious and not long-term use of the drug. Dobutamine acts directly on β1 receptors, very weak with α1 and β2 receptors, so it causes less heart rate increase, less arrhythmia than other catecholamines.
Some notes when using Dobutamin inotropic drugs are:
Before using dobutamine, must compensate for enough circulating volume. The drug can cause skin necrosis, inflammation at the injection site, and the drug is absorbed. During drug administration, it is necessary to closely monitor the electrocardiogram, blood pressure and cardiac output, pulmonary pressure. Dobutamine should be used with extreme caution after myocardial infarction. Dobutamine concentrate should be diluted before use
1.3. Dopamine
Dopamine directly stimulates α1, α2, β1 - adrenergic receptors, and indirectly releases noradrenalin from the terminals of sympathetic and postganglionic sympathetic nerves, autonomic ganglia produces many different effects . On the heart, dopamine has the effect of increasing myocardial contractility, increasing blood flow and increasing stroke volume. At low or moderate doses, Dopamine does not cause tachyarrhythmias.
Dopamine is indicated as an anti-shock drug due to myocardial infarction, trauma, sepsis and cardiac surgery when cardiopulmonary resuscitation is required. Dopamine has the advantage in the treatment of acute renal failure with reduced renal perfusion or oligouria. However, it should be noted that in order for dopamine to work, it must first be infused with fluids to compensate for the decrease in blood volume. Clinically, Dopamine is widely used in the treatment of acute congestive heart failure and chronic decompensated heart failure unresponsive to digoxin and diuretics.
Some notes when treating with Dopamine are:
Before starting treatment with Dopamine, it is necessary to compensate for hypovolemia. During treatment with Dopamine, it is necessary to closely monitor cardiovascular parameters such as central venous pressure, blood pressure, urine output, etc. In the case of patients with peripheral arterial diseases such as: In Raynaud's syndrome, diabetic endocarditis, Buerger's disease or other vascular disease, dopamine should be started at a low dose, then increased gradually. During Dopamine infusion, patients may experience vasoconstriction, especially at high doses. Dopamine has an advantage in the treatment of acute heart failure due to decreased myocardial contractility. However, when outflow is obstructed (in aortic or pulmonary stenosis, etc.), cardiac output may be reduced when dopamine is given, because of increased afterload. Prevention of the risk of myocardial infarction due to vasoconstriction can occur even with low doses of Dopamine. Dopamine should be used with caution in patients with liver failure.
Thuốc Dopamin có tác dụng tăng co bóp cơ tim
1.4. Noradrenaline
Noradrenalin has completely similar properties to endogenous catecholamines synthesized by the adrenal medulla and sympathetic nervous tissue. Noradrenalin is a β- and α-receptor agonist that increases heart rate, increases myocardial contractility, and increases peripheral vasoconstriction. The noradrenaline is indicated in the case of septic shock; heart shock. This is a drug used in combination in cardiac arrest with low blood pressure.The notes when using Noradrenalin inotropic drugs are:
Be careful when using the drug for patients with hypertension, hyperthyroidism, young children; the patient is taking tricyclic antidepressants and MAO inhibitors. If concentrated infusion of Noradrenalin can cause severe tissue irritation, only diluted solutions should be administered, and if possible, central intravenous or large vessels should be administered. The usual dose of noradrenaline is 0.2 to 1 mcg/kg/min. Like other vasopressors, noradrenaline can cause side effects such as tachycardia, myocardial ischemia and arrhythmia,...
2. Non-Adrenergic inotropic drugs
2.1. Milrinone
Milrinone is an inotropic agent that has been used clinically for the treatment of severe heart failure since the 1990s. Milrinone belongs to the bipyridine class of drugs, has an inotropic effect, is used for intravenous infusion in patients with severe left ventricular dysfunction. Because Milrinone helps to relax the left ventricle, it is very beneficial for patients with diastolic heart failure. Along with that, Milrinone also has advantages for patients with heart failure who have elevated pulmonary artery pressure. By relaxing the smooth muscle on the pulmonary artery wall, Milrinone helps reduce pulmonary artery pressure and improve right ventricular function.
Precautions when using the inotropic agent Milrinone are:
Milrinone can cause hypotension, especially when the ventricular filling pressure is low. Caution is advised when prescribing milrinone to patients with renal impairment because milrinone is eliminated by the kidneys. The half-life of milrinone is relatively long (more than 50 minutes) so if there are side effects such as hypotension or cardiac arrhythmias these side effects can last for hours. Intravenous bolus milrinone can cause severe hypotension and should not be used.

Milrinone có thể gây hạ huyết áp ở một spsp trường hợp
2.2. Levosimendan
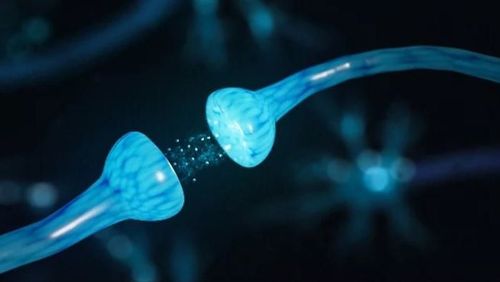
Levosimendan drug increases the sensitivity of troponin C to intracellular calcium, thereby increasing the contractility and relaxation of the myocardium. Levosimendan also induces peripheral vasodilation by opening up adenosine triphosphate (ATP)-dependent potassium channels on the surface of smooth muscle cells. The drug works quickly, the symptoms are improved immediately. In hemodynamically impaired heart failure patients, the efficacy of the inotropic agent levosimendan is dose dependent. Usually, a dose adjustment should be made every 4 hours from 0.1 mcg/kg/min to 0.4 mcg/kg/min and maintained at this dose for the following hours. Several studies have shown that Levosimendan helps improve patients' quality of life.
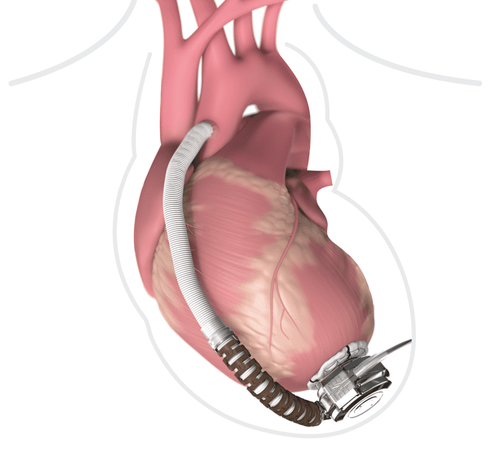
Besides the inotropic drugs that have been used for a long time as above, new generations of drugs are continuing to be researched and developed. Some promising drugs such as Omecamtiv mecarbil, Istaroxime,... not only increase myocardial contractility, have few side effects, but also improve mitochondrial function through regulation of the regeneration process. biological generation, oxidation in cells, ion exchange,...
Vinmec International General Hospital is the address for examination, treatment and prevention of diseases. When performing the examination process at Vinmec, customers will be welcomed and used modern facilities and machinery along with perfect medical services under the guidance and advice of doctors. Good doctors, well-trained both at home and abroad.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.