This is an automatically translated article.
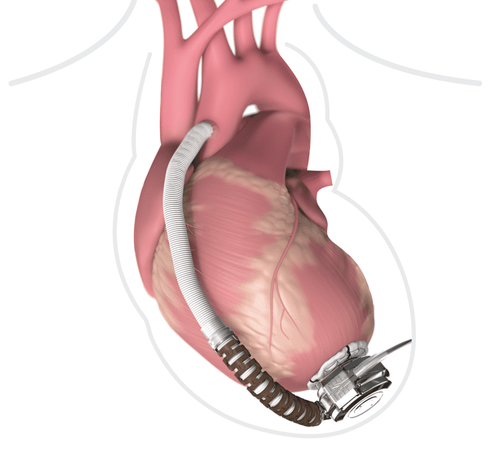
The article is professionally consulted by Master, Doctor Huynh Khiem Huy - Cardiac Resuscitation Doctor - Cardiovascular Center - Vinmec Central Park International General HospitalAcute heart failure is a complex clinical syndrome. Most patients with acute heart failure admitted to the hospital have fluid overload, signs of blood stasis, or may experience hypotension and organ hypoperfusion.
1. Classification of acute heart failure
Acute heart failure due to hypertensive crisis Acute coronary syndrome with heart failure Acute pulmonary edema Cardiogenic shock Acute decompensated heart failure Right heart failure2. Symptoms and physical symptoms of acute heart failure with acute pulmonary edema
2.1. Symptoms The patient suddenly feels short of breath, hungry for air, coughs, spits up pink foam, drowns. Patients often have to sit up and do not speak enough sentences Breathing rate increases, respiratory muscle contractions Sweating, cyanosis
Suy tim cấp gây ra các triệu chứng ho, khó thở cho người bệnh
3. General management of acute heart failure
3.1. At the primary level Symptomatic treatment Provide oxygen Improve organ perfusion and hemodynamics Avoid heart and kidney damage Prevent venous thrombosis Reduce ICU stay 3.2. In cardiology Have a reasonable treatment strategy Provide initial therapy Find causes and predisposing factors
Người bệnh suy tim cấp cần được xử trí và điều trị kịp thời
4. Management of acute pulmonary edema
4.1. Use of diuretics Depends on the patient's fluid retentionModerate: 20-40mg furosemide orally or intravenously Severe: 40-100mg furosemide intravenously, may increase dose or 5-40mg/h furosemide IV In case of poor response to furosemide: Add 50-100mg of thiazides in combination with furosemide, the effect is better than increasing the high dose of furosemide or 25-50mg of spironolactone in combination with furosemide if there is no renal failure In case of poor response to furosemide and thiazides: Add dopamine or dobutamine. Consider dialysis or ultrafiltration in patients with renal failure. 4.2. Give oxygen as soon as possible Goal: raise SpO2 >= 95% (>90% in COPD patients)

Người bệnh cần được thở oxy trong xử trí và điều trị phù phổi cấp

Một số loại thuốc tim mạch được bác sĩ áp dụng trong phác đồ điều trị bệnh
Master. Dr. Huynh Khiem Huy has more than 11 years of experience working in the field of cardiovascular resuscitation anesthesia; examination and resuscitation treatment after surgery for cardiovascular diseases in adults and children. Dr. Huy was former deputy head of the Department of Surgical Resuscitation at Tam Duc Heart Hospital before being a cardiothoracic surgeon in Cardiovascular Surgery, Cardiovascular Center - Vinmec Central Park International General Hospital
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
The article references the source: Vietnam Association of Vietnamese Studies