Genetic studies have demonstrated that uterine fibroids are monoclonal tumors originating from uterine smooth muscle stem cells, which undergo specific molecular changes, transforming into tumor-initiating stem cells that proliferate and differentiate under the influence of steroid hormones. There has been growing interest in the role of micronutrients, including vitamins, in the treatment of uterine fibroids. This article will delve further into this topic.
1. Uterine fibroids
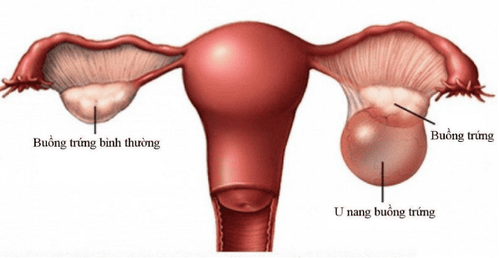
Uterine fibroids, also known as leiomyomas, are muscular tumors that can develop in or on the uterus. They rarely become cancerous, and having uterine fibroids does not significantly increase the risk of uterine cancer.
Fibroids can vary in size, shape, and location. They may develop inside the uterine cavity, within the uterine wall, or on the surface of the uterus. Fibroids may also attach to your uterus by a stalk-like structure or stem.
Some fibroids are small enough to be undetectable to the eye. While others grow into large masses that can distort the size and shape of the uterus.
Uterine fibroids typically occur in women of reproductive age, particularly between 30 and 40 years old, though they can appear at any age.
2. Causes of uterine fibroids
The exact cause of uterine fibroids is unclear, but hormonal and genetic factors are thought to play significant roles:
- Hormonal factors: Estrogen and progesterone, the hormones responsible for thickening the uterine lining during the menstrual cycle, also seem to stimulate fibroid growth. Fibroids often shrink after menopause when hormone levels decline.
- Genetic factors: Research has shown genetic differences between fibroids and normal uterine cells.
- Other growth factors: Substances like insulin-like growth factor, which helps maintain tissues, may influence fibroid development.
- Extracellular matrix (ECM): Extracellular matrix enables your cells to adhere to each other. Fibroid tumors contain more extracellular matrix than normal cells, which causes them to become fibrous. The extracellular matrix also retains growth factors within it, leading to cellular changes.
3. Risk factors
Several factors may increase the risk of developing uterine fibroids, including:
- Age
- Ethnicity
- Early onset of menstruation
- Using birth control
- Vitamin D deficiency
- High consumption of red meat and low intake of green vegetables, fruits, and dairy products.
- Alcohol use
- Family history
You are more likely to get uterine fibroids if your mother or sister has had uterine fibroids.

4. Diagnosis of uterine fibroids
Uterine fibroids are often discovered during routine pelvic exams. If abnormalities in the size or shape of the uterus are detected, further diagnostic tests may be required:
- Ultrasound: Ultrasound uses sound waves to capture images of the uterus. The technician places an ultrasound device either inside your vagina or on your abdomen to obtain the images. These images allow the doctor to determine whether you have uterine fibroids, as well as their size, location and characteristics.
- Blood tests: The doctor may recommend blood tests to determine the cause of your uterine fibroids. A complete blood count (CBC) can determine whether you have anemia (a low red blood cell count) or other bleeding disorders.
- Magnetic resonance imaging (MRI): In case the doctor requires additional information after your ultrasound, you may also undergo an MRI scan. MRIs show more detailed images of fibroids and can assist the doctor in determining the most appropriate treatment options. The doctor may also recommend an MRI scan if you have an enlarged uterus or are approaching menopause.
- Hysterosonography: In this procedure, saline is injected into the uterine cavity to expand it. This allows them to visualize fibroids growing within the uterus (submucosal fibroids) as well as the uterine lining. This technique is particularly useful if you are trying to conceive or experiencing heavy menstrual bleeding.
- Hysterosalpingography: to check whether the fallopian tubes are blocked, you may undergo a hysterosalpingography procedure. During this test, the doctor uses a contrast dye to highlight the uterus and fallopian tubes on X-ray images, allowing for better visualization of these areas.
- Hysteroscopy: the doctor inserts a small, lighted telescope-like device into your cervix. Then, saline is injected to expand the uterine cavity, allowing the doctor to examine the uterine walls and the opening of your fallopian tubes.
5. Treatment of Uterine fibroids
The most appropriate treatment depends on the severity of symptoms, desire for future pregnancies, age, and fibroid location.
Watchful waiting
If you have only mild symptoms or no symptoms at all, your doctor may recommend waiting. Fibroids are not cancerous, and they grow slowly or not at all. Because fibroids can also shrink or disappear after menopause.
Medications
Medications aim to manage symptoms rather than eliminate fibroids. Some medications may reduce the size of fibroids or alleviate pain and bleeding:
Oral contraceptives: Can reduce heavy bleeding.
Nonsteroidal anti-inflammatory drugs (NSAIDs): Help manage pain.
What vitamins should not be used for uterine fibroids?
Vitamins A and D are of particular interest following studies of their effects on treating uterine fibroids, while vitamins B3, C, and E have not been extensively studied. However, vitamins, especially vitamin D, and iron supplements may help provide energy if you have heavy bleeding and are anemic.

Other medications include:
- Oriahnn, a combination of elagolix, a GnRH antagonist, estrogen, and progestin, the first nonsurgical oral medication approved by the FDA to control heavy menstrual bleeding. Taking it can reduce bleeding by an average of 50%
- Gonadotropin-releasing hormone (GnRH) agonists, which temporarily induce menopause by blocking estrogen and progesterone. This can shrink your fibroids.
A progestin-releasing intrauterine device (IUD) inserted into the uterus can help control heavy bleeding. It also helps prevent pregnancy.
Tranexamic acid (Cyklokapron, Lysteda) is a non-hormonal medication. You take it on heavy bleeding days to slow your flow.
Surgical options
For moderate to severe symptoms, surgery may be necessary:
- Myomectomy: Removes fibroids while preserving the uterus, suitable for women planning future pregnancies.
- Endometrial ablation. A surgeon uses a laser or freezing to remove or destroy the lining of your uterus. You can have this procedure as an outpatient. Usually, you will stop having periods after that date and you will not be able to get pregnant again.
- In a procedure called uterine fibroid embolization (UFE), or uterine artery embolization (UAE), your doctor blocks the blood flow to the fibroids by inserting gel or plastic beads into nearby blood vessels. This causes the fibroids to shrink.
- Hysterectomy: This surgery completely removes your uterus, which is the only way to completely cure fibroids. The surgery is major, but your doctor has options for how to do it, including cutting through your abdomen or even laparoscopically.
6. Prevention of uterine fibroids
Fibroids can’t be prevented, but some research suggests that certain lifestyle habits may reduce your chances. A diet high in sugar may lead to a higher risk for some women. Consuming fresh fruits and cruciferous vegetables such as arugula, broccoli, cabbage, cauliflower, collard greens, and turnip greens may reduce your risk. Cruciferous vegetables are rich in nutrients such as beta-carotene, folate, vitamins C, E, K, and other minerals. They’re also packed with fiber. Evening primrose oil may help balance hormones for those at risk of fibroids. As for soy, more research is needed to prove its role in supporting fibroids.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: ncbi.nlm.nih.gov, webmd.com