This is an automatically translated article.
The article was professionally consulted with Specialist Doctor II Dinh Van Loc - Department of General Surgery - Vinmec Danang International General Hospital.The role of the anesthesiologist has evolved from that of a physician primarily concerned with providing optimal surgical conditions and minimizing pain immediately after surgery, to a perioperative physician who is responsibility for ensuring optimal management of surgical patients before, during, and after surgery
Most women who have a caesarean section share that, during the process of caesarean section, surgical stitches they feel lightly. What scares them most is the pain after giving birth, the pain is unbearable, the pain is unbearable. Post-operative pain makes many mothers unable to take care of themselves in hygiene activities, unable to breastfeed. If not treated, the acute pain after surgery will turn into chronic pain, and cause post-operative depression.
Therefore, the job of an anesthesiologist is to anesthetize during surgery and resuscitate after surgery. In order to minimize pain and inconvenience in daily life, the anesthesiologist will advising women on methods of pain relief after cesarean section by multimodal analgesia. At VINMEC hospitals, we always carry out routine post-operative pain relief procedures according to international standards.

1. Overview
Treatment of pain after cesarean section is important because it affects the recovery of the mother. Although new modalities of analgesia and analgesia have developed in recent years, the present shows that we are far from achieving the goal of optimal postoperative pain relief. Pain relief is an integral and necessary component of any procedure or surgery, and a cesarean section is no exception. Pain ranks highest among adverse clinical outcomes associated with cesarean section. Patients after cesarean section often experience moderate to severe pain in the postoperative period. If this pain is not adequately treated, it can interfere with child care, breastfeeding and also increase the mother's risk of depression and lead to chronic pain syndrome.Definitions and related concepts:
Cesarean section: is a surgery to remove the fetus, placenta, amniotic membrane by an incision through the abdominal wall and uterine wall intact. Pain after cesarean section is the pain of the incision and pain caused by uterine contractions. Mastering effective pain relief and pain treatment methods for women after cesarean section. Ensure patient safety. Pregnant women do not have pain after surgery, do not use Opioids after surgery.

2. Advantages and disadvantages of pain relief after cesarean section
After cesarean section, women often face pain. It is due to disorders of the respiratory, circulatory, endocrine organs. When the anesthetic wears off, the incision will make the mother feel very painful. The mother could only lie still on the bed, not daring to move, or turn. The continuous infusion of anesthetic into the nerve trunk, reducing pain in the upper and lower extremities helps pregnant women reduce pain after cesarean section.Treatment of pain after cesarean section is very important because it affects the recovery of the mother. Although new modalities of analgesia and analgesia have developed in recent years, the present shows that we are striving to achieve the optimal goal of postoperative pain relief.
Pain relief is an integral and necessary component of any procedure or surgery, and a cesarean section is no exception. Pain ranks highest among adverse clinical outcomes associated with cesarean section. Patients after cesarean section often experience moderate to severe pain in the postoperative period. If this pain is not adequately treated, it can interfere with child care, breastfeeding and also increase the mother's risk of depression and lead to chronic pain syndrome.
2.1. Advantage
Bilateral squamous sphincter anesthesia:Lumbar squamous sphincter anesthesia is also evaluated for good pain control after cesarean section. The analgesia of lumbar sphincter after cesarean section was also evaluated by a randomized controlled trial, and the results demonstrated statistically better morphine demand and consumption in the squamous muscle group. waist compared with the control group. A recent randomized controlled trial also found effective pain relief in cesarean section compared with a control group.
The exact mechanism of action and analgesia of lumbar squamous sphincter is also not fully understood. However, it is thought to be due to paraspinal spread and the effect of the anesthetic on sympathetic fibers in the lumbar region. Safety is another concern in lumbar sphincteric anaesthesia, because of its deep blockade and close proximity to the kidney and other intraperitoneal visceral organs to ensure safety of anesthesia. Vinmec Hospitals we always perform anesthesia under ultrasound guidance, the team of doctors is continuously trained and proficient with this technique. Recently, spinal anesthesia has been shown to effectively reduce pain after cesarean section; however, only a few case reports have been published and clear evidence of effectiveness has yet to be provided.
Anesthesia for both sides of the lumbar squamous muscle in combination with Catheter for pain relief at the incision
Placement of an analgesia catheter at the incision; right at the incision, between the peritoneum and the muscle fascia. Catheter holes should cover the entire length of the incision. Fix the foot of the percutaneous catheter with thread. Anesthesia 0.2% Anaropine used in automatic continuous pump at 4-5ml/h starts running pain reliever after 30 minutes of lumbar squamous sphincter, continuously up to 48 hours after surgery.
Epidural anesthesia has an effective route of pain relief. Before the caesarean section began, the woman was placed in a catheter to infuse an epidural and analgesia. If analgesia is desired after a cesarean section, the catheter will be kept and an appropriate dose of local anesthetic infused.
The method of pain relief after cesarean section with epidural anesthesia is evaluated for safety. It has a good analgesic effect, especially when the mother takes a deep breath, coughs or moves in bed. It does not affect life function, has very few unwanted effects compared to other pain relief methods. Maintain effective pain relief after cesarean section from 24 to 72 hours. Pregnant women can exercise early to avoid thrombosis after surgery. In particular, because there is no pain, it will help pregnant women recover function effectively. Routine pain assessment and analgesia for the mother are also given due attention. Analgesia alone is not sufficient in patients with cesarean section. In addition to analgesia, optimal management of the patient after cesarean section should pay attention to the goal and unrestricted maternal mobility, minimal maternal and neonatal side effects, and rapid functional recovery. basic functions and early discharge from hospital. Existing pain relief techniques have attempted to address these problems. Furthermore, the availability of drugs and trained medical professionals play an important role in the selection of pain relief methods and the quality of pain relief, which is an advantage we now bring to life. patient safety and satisfaction

3. Some influencing factors
The severity of pain after cesarean section is multifactorial, and the current universal approach is not appropriate for all women, due to individual differences in pain perception and other factors. other affect pain. Although many tools have been developed to help predict pain severity, effective pain control remains a challenge for patients after cesarean section. Injectable opioids, though widely used, often provide inadequate pain relief, and opioid-related side effects can lead to mothers becoming opioid dependent. Neural administration of opioids provides effective analgesia after cesarean section, but the duration of analgesia is short and the patient often requires additional analgesia. The inherent limitations of the previously used technique and the individual variability of postoperative pain make it difficult to achieve effective analgesia in the cesarean section patient.
4. Some recommendations for using multimodal analgesia for pain relief
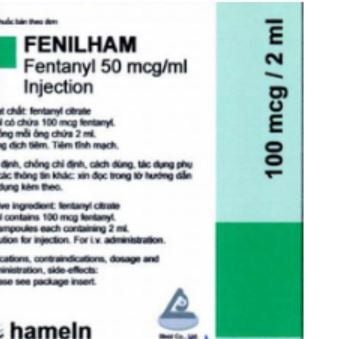
To overcome the limitation in providing effective analgesia during cesarean section, the current recommendation to use multimodal analgesia for analgesia. In multimodal analgesia, the simultaneous use of more than two drugs or techniques with different mechanisms of action to provide effective analgesia. The goal of multimodal analgesia is to obtain synergistic or additive analgesia with fewer side effects by combining smaller amounts of each drug with different mechanisms of action. Multimodal analgesia includes the use of non-steroidal anti-inflammatory drugs, paracetamol, topical wound infiltration, spinal and epidural opioids, and the use of horizontal anesthesia of the transverse abdominal or inferior lumbosacral muscles. ultrasound guide. Injectable opioids are reserved for those who do not respond to the above methods or treat severe acute pain.When non-steroidal anti-inflammatory drugs are used together with CNS opioids for pain relief during cesarean section, the maternal need for opioids is reduced and its side effects are reduced. In this synergistic effect, nonsteroidal anti-inflammatory drugs relieve visceral pain and opioids relieve wound pain. However, nonsteroidal anti-inflammatory drugs must be used with caution because of potential problems with bleeding, platelet dysfunction, and kidney failure.
Multimodal analgesia is the standard recommendation of the current international anti-anxiety association for postoperative pain relief.. Currently, our Vinmec system hospitals have access to the above new techniques, have enough drugs, enough human resources to effectively treat pain, evaluate and monitor each woman after cesarean section, and always adhere to the regimen and continuously improve in the process of caring for pregnant women. The anesthesiologist must play a key role in the planning of postoperative analgesia regimens, and each post-cesarean section woman must receive good analgesia, and be assessed and planned for an adequate analgesia by the anesthesiologist. of the vimec system.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.