This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalEsophageal motility disorders (EMD) represent a diverse group of conditions that alter the normal movement and movement of food from the esophagus into the stomach. The most common symptoms include difficulty swallowing and chest pain. Difficult to distinguish from other common diseases such as coronary artery disease, gastroesophageal reflux disease and malignancy.
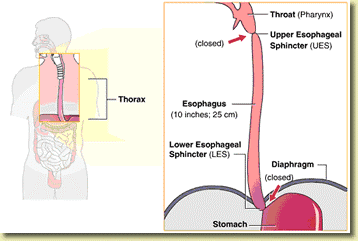
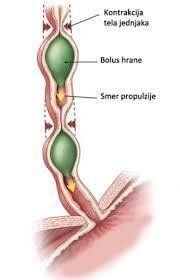
1. Esophageal movement and swallowing
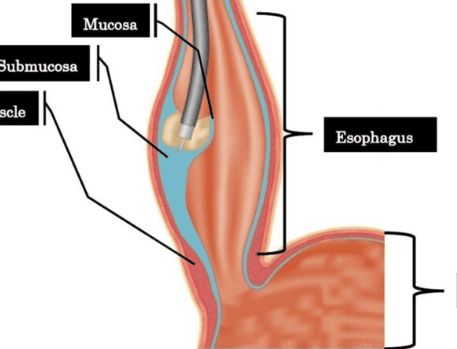
Organs involved in swallowing include the pharynx, the upper esophageal sphincter (crispharyngeal muscle), the esophageal body, and the lower esophageal sphincter (LES) of the upper third of the esophagus, as well as other structures. the periphery is composed of striated muscle fibers; The distal esophagus and LES are composed of smooth muscle fibers. These ingredients act as an integrated system that helps move food from the mouth to the stomach and prevents it from backing up into the esophagus. Mechanical obstructions and disorders that interfere with motor function (esophageal motility disorders) can affect the upper system.Patient history may suggest diagnosis in 80% of cases. Symptoms found on examination in esophageal disorders include cervical and supraclavicular lymphadenopathy due to metastases, neck swelling due to pharyngoesophageal diverticulum or thyroid enlargement, white patches at the back of the mouth- pharyngeal candidiasis, and prolonged swallowing time (time from swallowing to hearing sound of liquid and air entering the stomach - normal ≤ 12 seconds when stethoscope is placed in the epigastrium). Observing the patient's swallowing process can help detect regurgitation of the nasal passages and airways. Most esophageal disorders require specific tests to make a diagnosis.
2. An overview of esophageal motility disorders (EMD)
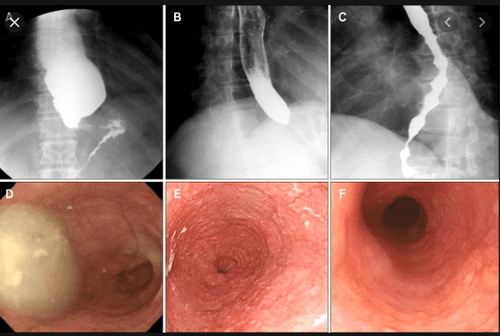
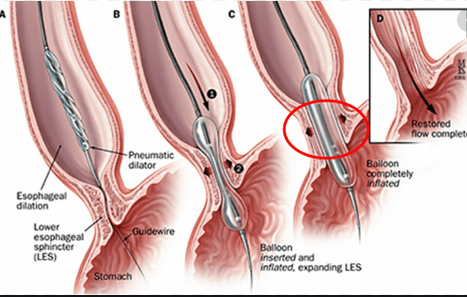
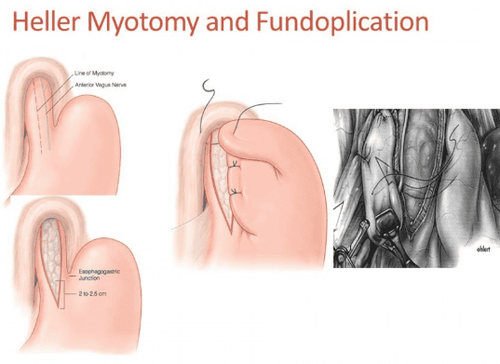
Esophageal motility disorders (EMD) represent a diverse group of conditions that alter the normal movement and movement of food from the esophagus into the stomach. The most common symptoms include difficulty swallowing and chest pain. Difficult to distinguish from other common diseases such as coronary artery disease, gastroesophageal reflux disease and malignancy.The most clearly and fully described esophageal motility disorder is achalasia, which causes increased esophageal motility and poor relaxation of the lower esophageal sphincter (lower esophageal sphincter). Treatment for esophageal motility disorders focuses on reducing the pressure of the lower esophageal sphincter to allow gravity to allow food to pass through the stomach. Balloon dilation and endoscopic Heller myotomy (LHM) with aneurysm reconstruction are standard treatments for esophageal motility disorders.
2.1 Clinical Manifestations of Esophageal Dysfunction The classic presenting symptom of achalasia is difficulty swallowing larger solids than liquids, often occurring for many years before being diagnosed. Patients often learn to adapt to dysphagia by changing their diet or performing exercises that improve swallowing. Dysphagia is often accompanied by easy regurgitation of poorly digested food or liquids and is often worse in the supine position or after eating several meals. Sometimes regurgitation can lead to aspiration pneumonia.
Dysphagia and weight loss are common symptoms of achalasia but are also primary malignancies of the esophageal or gastroesophageal junction. Gastroesophageal junction malignancy can cause rapid weight loss and difficulty swallowing and is called pseudo-achalasia. These symptoms may also be seen in esophageal stricture, esophagitis, esophageal ulceration, or extrinsic compression from mediastinal masses.
Drug therapy Pharmacotherapy to lower esophageal sphincter pressure is currently limited to nitrates such as isosorbide dinitrate and calcium channel blockers such as diltiazem or nifedipine. These drugs can reduce pressure and improve swallowing in some patients. However, side effects such as dizziness, stagnation, and hypotension would limit their use in this population. Noncardiac chest pain in spastic esophagitis may respond to treatment with tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs). These medications can also often successfully treat the anxiety that often accompanies these disorders. The lowest dose should be used to successfully treat chest pain.
Proton pump inhibitors (PPIs) and H2-receptor antagonists have essentially no role in the treatment of esophageal motility disorders. Acid reflux does not readily occur in patients with achalasia who have a hypertensive lower esophageal sphincter. Patients with Esophageal Dysfunction and normal lower esophageal sphincter pressure (normal IRP above HRM) may occasionally develop GERD and therefore rarely have esophagitis that may respond to antisecretory therapy. . The diagnosis of GERD can often be elucidated by upper endoscopy but may require formal esophageal pH testing or assessment of response to PPI therapy for an accurate diagnosis.
Endoscopic intervention Injecting botulinum toxin into the hypertensive lower esophageal sphincter or spastic esophageal muscle during upper endoscopy has been used for decades to treat esophageal motility disorders. Botulinum toxin is an inhibitor of acetylcholine release from nerve cells and when administered to the esophageal body or the lower esophageal sphincter, it reduces contraction amplitude and sphincter pressure respectively. The standard injection dose is 80-100 units in four quadrants about 1-2 cm above the lower esophageal sphincter.
This leads to rapid improvement in about 80% of patients with achalasia. However, at 12 months after injection, only 40-50% of patients maintain a response and require booster injections to maintain efficacy. Therefore, treatment of lower esophageal sphincter pressure (achalasia or EGJOO) with botulinum toxin in 2019 is intended for diagnostic purposes or for patients who prefer or are at high risk for laparoscopic surgery. (eg elderly people with comorbidities). For spastic esophagitis, injection of 100 units of botulinum toxin into the middle or distal esophagus may relieve chest pain but similarly requires repeated treatment in most patients to maintain response.
Surgery The standard surgical procedure for achalasia is laparoscopic Heller myotomy (LHM). This procedure creates a 3-cm myotomy through the lower esophageal sphincter on the anterior wall of the lower and upper esophagus of the stomach. This muscle ablation is performed in most patients with an aneurysm to reduce the risk of post-procedural reflux. Many long-term studies demonstrate the effectiveness of LHM in 85-90% of most patients.
3. Conclusion
Under normal circumstances, esophageal motility occurs in a coordinated, sequential manner to push food into the stomach. Esophageal motility disorders represent a diverse group of conditions that alter this movement of the esophageal or lower esophageal sphincter. The most common symptoms include difficulty swallowing and chest pain. Difficult to distinguish from other common diseases such as coronary artery disease, gastroesophageal reflux disease and malignancy. Standard work includes upper gastrointestinal endoscopy, barium esophagography, and high-resolution esophageal manometry. Treatment of achalasia focuses on reducing the pressure of the lower esophageal sphincter. Balloon dilation and laparoscopic Heller myotomy are the most commonly used treatments. Oral endoscopic myotomy (POEM) represents the newest endoscopic treatment option, and early data suggest comparable efficacy to Heller myotomy. As diagnostic and therapeutic options for esophageal motility disorders are increasing, a multimodal approach is required and referral to gastroenterology or surgery is recommended for further management of these disorders.Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, gastric mucosa Esophageal ectopic... Along with that, at Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow) function. Banding Imaging - endoscopy with narrow light frequency) results in clearer images of mucosal pathology than conventional endoscopy, detecting ulcerative colitis lesions, digestive cancer lesions In the early stages... Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can be assured of endoscopy services. stomach, esophagus at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: John Dewitt, update in the diagnosis and treatment of esophageal motility disorders, Dispatches from the guild conference, series20, practicalgastro, march 2019 • volume XLIII, issue 3