This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalExtraesophageal manifestations associated with gastroesophageal reflux disease are frequent and represent a diagnostic and therapeutic challenge. Two main mechanisms have been proposed to explain the extraesophageal manifestations associated with gastroesophageal reflux disease: direct injury to gastric contents and indirect, mediated injury. vagus nerve.
1. Gastroesophageal reflux disease overview
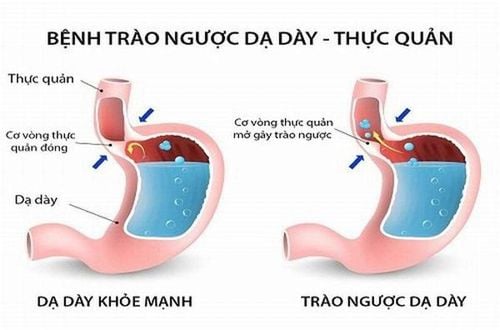
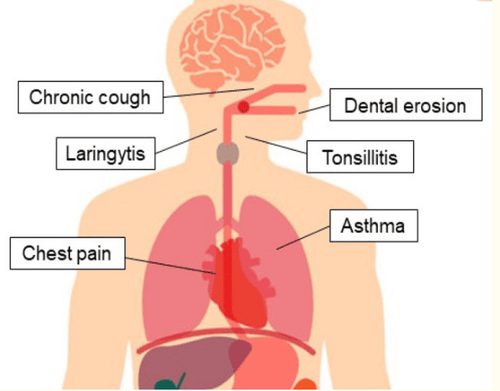
Gastroesophageal reflux disease (GERD) is a common gastrointestinal (GI) disease worldwide and has a high prevalence in Western countries. The 2006 Montreal Consensus defined gastroesophageal reflux disease as a condition that develops when the reflux of gastric contents causes troubling symptoms and/or complications into the esophagus.Extraesophageal manifestations associated with gastroesophageal reflux disease are frequent and represent a diagnostic and therapeutic challenge, possibly involving the lungs, upper respiratory tract, and mouth, presenting with asthma , laryngitis , chronic cough , tooth wear and noncardiac chest pain .
2. Mechanism of extraesophageal manifestations related to gastroesophageal reflux disease
2 main mechanisms have been proposed to explain the extraesophageal manifestations associated with gastroesophageal reflux disease: direct injury to gastric contents and indirect, cord-mediated injury. vagus nerve.In the direct stimulus hypothesis, cough, laryngitis, or exacerbation of asthma occurs due to reflux of fluid into the trachea or bronchi, irritating the pharynx and larynx. An intact lower esophageal sphincter (LES) and superior esophageal sphincter protect against gastroesophageal reflux, while the high basal pressure of the upper esophageal sphincter and the esophagoglottic closure reflex prevent prevent contact of the pharynx and larynx with the refluxed substance. The indirect mechanism hypothesis is based on a common embryonic origin and vagal innervation of the esophagus and bronchial tree, considering cough, bronchospasm, and cardiogenic chest pain due to stimulation of the bronchial reflex arc. from distal esophageal reflux.
2.1 Pulmonary manifestations Several epidemiological studies have suggested an association between gastroesophageal reflux disease and asthma in particular, and respiratory symptoms in general, although a causal relationship has not been established. proven. Here, we discuss the most frequently reported pulmonary manifestations of gastroesophageal reflux disease: Chronic cough, asthma, and aspiration pneumonia.
2.2 Chronic Cough Cough is defined as chronic when it lasts more than 8 weeks; A much more persistent cough is defined as a chronic cough that is intractable. Common causes of chronic cough are side effects from commonly used medications (especially ACE inhibitors), tracheomalacia, chronic obstructive pulmonary disease (COPD), bronchiectasis. , asthma, obstructive sleep apnea, meningitis, and gastroesophageal reflux disease. In non-smoking, normal chest X-rays without ACE inhibitors, chronic cough was identified in 86% of cases as asthma, postnasal drip syndrome (PNDS), and GERD, although often multiple causes coexist.
Diagnosis of Chronic Reflux Cough Coughs caused by gastroesophageal reflux disease are often dry and often aggravated by changes in posture, food intake, and phonetics. Chronic cough is often the only manifestation of gastroesophageal reflux disease. In patients presenting with a chronic cough, lung disease should first be ruled out by performing a radiological examination, such as a chest x-ray or computed tomography (CT) of the lungs. Some cases require bronchoscopy for diagnostic or therapeutic reasons.
When gastroesophageal reflux disease causes cough due to irritation of the larynx, laryngoscopy may demonstrate findings consistent with "reflux laryngitis". During bronchoscopy, abnormalities consistent with aspiration can be detected, such as sublaryngeal stenosis, tracheobronchial hemorrhage, and congestion of the accessory bronchi. Evidence of inflammation and edema of the larynx and lower airways should not automatically translate to gastroesophageal reflux disease as these findings may be related to other causes of cough or to the cough itself. . If imaging and endoscopy are normal, it can be assumed that gastroesophageal reflux disease causes cough by stimulating the esophageal-bronchial reflex. In GERD, there are many potential cough mediators other than acid, so several possible mechanisms are suggested.
Treatment of Reflux Cough Although there is little evidence to support this approach, PPIs are the most common treatment used in cases of suspected chronic cough due to gastroesophageal reflux disease. Several studies have shown improvement of chronic cough with this treatment; however, a recent randomized controlled trial (RCT) did not show a difference between PPIs and placebo. Explanation can be found in the small sample size included and in the types of quality of life (QoL) questionnaires used to address the usefulness of treatments.
Gastroesophageal reflux is suggested as a cause of asthma, as well as when clinically silent, and an effective reflux treatment may improve asthma control.
Similarly, given the challenges encountered in chronic cough, the diagnosis of asthma associated with gastroesophageal reflux disease is difficult: upper endoscopy, pH impedance and PPI testing when positive An association between diseases has not always been demonstrated. Silent reflux and nocturnal regurgitation are very common in patients with asthma and respiratory symptoms: during sleep, the usual protective responses are absent, increasing the damage caused by reflux.
Treatment of reflux asthma Lifestyle changes, such as elevating the head of the bed, stopping smoking, and dietary changes (reduced fat, chocolate, alcohol, citrus, tomatoes, coffee and drinking tea, avoiding large meals, and eating three hours before bedtime) are recommended to improve reflux control and may help improve bronchial symptoms, although there are no RCTs to confirm this hypothesis .
Although PPIs have demonstrated superiority over H2 blockers for the treatment of esophagitis, the efficacy of the former in the treatment of GERD-associated asthma remains questionable. debate: some studies reported improvement in symptoms and lung function with reflux treatment, while others did not demonstrate this effect.
2.4 Laryngitis Laryngo-pharyngeal reflux (LPR) is defined by the 2002 consensus of the American Academy of Otolaryngology Surgeons as a disorder of the backward flow of gastric contents into the larynx. and pharynx. This is a common extraesophageal presentation associated with gastroesophageal reflux disease: Up to 10–15% of all visits to ENT clinics are due to manifestations of laryngeal reflux- oropharyngeal
Gastroesophageal reflux disease can cause many symptoms in the larynx, such as hoarseness, pain or burning in the throat, pain when swallowing, feeling of lump in the throat, cough, throat clearing repetitive, profuse phlegm, difficulty swallowing and voice fatigue. These complaints are not specific to gastroesophageal reflux disease and laryngopharyngeal reflux disease, and they may also be caused by allergens, smoke, and various irritants.

2.5 Reflux Oral Pathology Saliva flow and swallowing function are significantly reduced in patients with gastroesophageal reflux disease. A decrease in saliva production leads to dry mouth, sometimes progressing to dry mouth disease. Gingivitis is defined as inflammation of periodontal soft tissue, which may result from decreased salivation. Coexistence of bruxism can exacerbate periodontal disease.
Dental Erosion Dental erosion is irreversible loss of tooth hard tissue by a chemical process unrelated to bacteria and it is a major known oral symptom of acid reflux in patients with GERD, according to the Montreal Definition and Classification. Prevalence Mean tooth erosion in patients with GERD varies widely, from 5% to 47.5%, with a higher severity than in healthy subjects.
Oral soft tissue disorders Oral soft tissue damage is one of the ENT diseases related to gastroesophageal reflux. Associations with gastroesophageal reflux disease have been suggested for tonsillitis, mucosal atrophy, congestion in the soft palate and uvula, glossitis, epithelial atrophy, lacrimal sac inflammation, and developmental disorders. Common oral complaints in patients with GERD are dry mouth, sour and sour taste, bad breath, itching and burning, and throat discomfort.
Gastroesophageal reflux disease can cause damage to the oral mucosa, although mucosal changes are not pathognomonic of gastroesophageal reflux disease: oral candidiasis, Sjögren's syndrome, dysuria Drug-associated diabetes, poor oral hygiene, dietary changes, and smoking-related oral lesions are also present. The Palatal regions are often destructive by gastroesophageal reflux disease.
2.6 Chest pain Chest pain associated with GERD is the most frequent atypical manifestation of GERD. Although the Montreal classification considers noncardiac chest pain an esophageal syndrome, we discuss it separately with the most common symptoms of typical GERD, such as heartburn and vomiting. regurgitation, due to similarities in diagnosis and treatment with extraesophageal manifestations.
Gastroesophageal reflux disease-associated chest pain is defined as recurrent posterior pain radiating to the back, neck, jaw, or arms, which can last from minutes to hours and is caused by exposure. with esophageal acidosis.

Differential diagnosis of chest pain associated with GERD disorders of the gut-brain interaction such as functional esophageal angina, reflux hypersensitivity, and functional heartburn. Esophageal motility disorders with an increase in the amplitude and duration of esophageal contractions, causing pain.
Visceral hypersensitivity is the proposed mechanism to explain noncardiac esophageal chest pain in cases of normal pH measurements. In these patients, non-pathological reflux (based on characteristics or duration) causes painful symptoms, such as heartburn or chest pain.
Gastrointestinal-Brain Interaction Disorders (DGBI) have been widely discussed in the Rome IV classification of functional disorders: They are defined as a group of disorders classified according to gastrointestinal symptoms associated with any combination of dyskinesia, visceral hypersensitivity, altered mucosal and immune function, gut microbiota, and/or central nervous system processing.
Treatment of chest pain associated with GERD represented by PPIs and H2 blockers, formerly considered primary first-line therapy. Patients with diagnosed gastroesophageal reflux disease (endoscopic findings and/or abnormal pH tests) improve symptoms in 78–92% of cases receiving antireflux therapy. In contrast, response to PPI treatment in patients with noncardiac chest pain without objective evidence of gastroesophageal reflux disease ranged from 10% to 14%. Furthermore, the duration of PPI therapy has not been elucidated, although a course of 2-3 months is generally recommended. On the other hand, failure to respond to the PPI trial for 2 weeks should lead to discontinuation of PPI therapy.
In summary, the diagnosis of extraesophageal manifestations associated with gastroesophageal reflux disease is not straightforward and is often excluded. Gastroesophageal endoscopy will help detect the disease early and take timely measures. Currently, Vinmec International General Hospital is one of the prestigious hospitals, trusted by a large number of patients for medical examination and treatment. Customers who choose gastroesophageal endoscopy at Vinmec will enjoy advantages such as:
Experienced doctors in endoscopy. Modern equipment, high treatment efficiency: C-Am system, intraoperative ultrasound machine helps to locate the position and help the surgeon to monitor the patient's condition during and after surgery. to be able to bring good endoscopic results, limit complications during and after surgery. Germany's most modern flexible endoscope system for clear, accurate images, easy to use. Intraoperative consumables are passed through strict sterilization testing procedures, Vinmec only uses high quality products and especially is used only once to ensure sterility and deliver results. good for the patient. With modern facilities, accurate diagnosis, selection of appropriate surgical methods, customers only take a single dose of prophylactic antibiotics, do not have to use high-dose antibiotics for a long time, no pain, no hospital stay. short, only 1-2 days. Therefore, saving treatment costs Professional services: Modern civilized disease prevention system, each patient one room is fully serviced from monitoring disease parameters, meals, rest regimes Rest, exercise, health education, each patient room is equipped with amenities like a hotel apartment, patient information is confidential.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesMarilena Durazzo,1,2,* Giulia Lupi, Extra-Esophageal Presentation of Gastroesophageal Reflux Disease: 2020 Update, J Clin Med. 2020 Aug; 9(8): 2559. Vakil N., Van Zanten S.V., Kahrilas P., Dent J., Jones R., Global Consensus Group The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus. Am. J. Gastroenterol. 2006;101:1900-1920. doi: 10.1111/j.1572-0241.2006.00630.x. [PubMed] [CrossRef] [Google Scholar]