This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Therapy for esophageal motility disorders initially focuses on the condition of the pressure in the lower esophageal sphincter. If the pressure is elevated, medical or surgical treatment is needed to reduce the pressure. In spastic motor disorders (jackhammer esophagus, type III achalasia, esophageal spasm), treatment may also focus on relaxing the esophageal muscle.
1. Medicines
Pharmacological therapy to lower esophageal sphincter pressure is currently limited to nitrates such as isosorbide dinitrate and calcium channel blockers such as diltiazem or nifedipine. These drugs can reduce pressure and improve swallowing in some patients. However, side effects such as dizziness, stagnation, and hypotension would limit their use in this population. Noncardiac chest pain in spastic esophagitis may respond to treatment with tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs). These medications can also often successfully treat the anxiety that often accompanies these disorders. The lowest dose should be used to successfully treat chest pain.
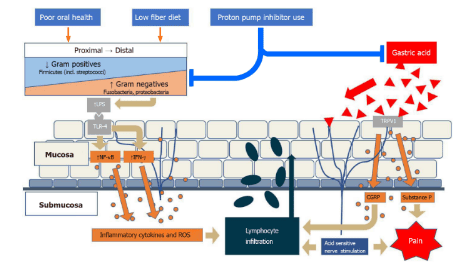
Proton pump inhibitors (PPIs) and H2-receptor antagonists have essentially no role in the treatment of esophageal motility disorders. Acid reflux does not readily occur in patients with achalasia who have a hypertensive lower esophageal sphincter. Patients with esophageal motility disorders and normal lower esophageal sphincter pressure (normal IRP above HRM) may occasionally develop GERD and thus rarely have esophagitis that may respond to antisecretory therapy. . The diagnosis of GERD can often be elucidated by upper endoscopy but may require formal esophageal pH testing or assessment of response to PPI therapy for an accurate diagnosis.
2. Endoscopic intervention
Injecting botulinum toxin into the hypertensive lower esophageal sphincter or spastic esophageal muscle during upper endoscopy has been used for decades to treat esophageal motility disorders. Botulinum toxin is an inhibitor of acetylcholine release from nerve cells and when administered to the esophageal body or the lower esophageal sphincter, it reduces contraction amplitude and sphincter pressure respectively. The standard injection dose is 80-100 units in four quadrants about 1-2 cm above the lower esophageal sphincter. This leads to rapid improvement in about 80% of patients with achalasia. However, at 12 months after injection, only 40-50% of patients maintain a response and require booster injections to maintain efficacy. Therefore, treatment of lower esophageal sphincter pressure (achalasia or EGJOO) with botulinum toxin in 2019 is intended for diagnostic purposes or for patients who prefer or are at high risk for laparoscopic surgery. (eg elderly people with comorbidities). For spastic esophagitis, injection of 100 units of botulinum toxin into the middle or distal esophagus may relieve chest pain but similarly requires repeated treatment in most patients to maintain response.
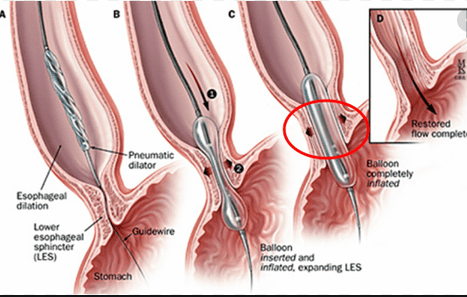
Endoscopic balloon dilation for esophageal stricture or achalasia uses balloons 30mm, 35mm, or 40mm in diameter, larger than those used to dilate typical esophageal strictures. During the procedure, the balloon is placed over the lower esophageal sphincter and gradually inflates leading to rupture of the sphincter muscles. Short-term treatment is effective in 85-90% of patients. However, after 12 months, only 60-70% remission is seen and repeat dilation is required for those who fail to respond. Complications of balloon dilation include chest pain in 10-15% and gastroesophageal perforation in 2-3% of patients. Perforation is usually treated conservatively by endoscopic closure or endoscopic stenting.
3. Surgery
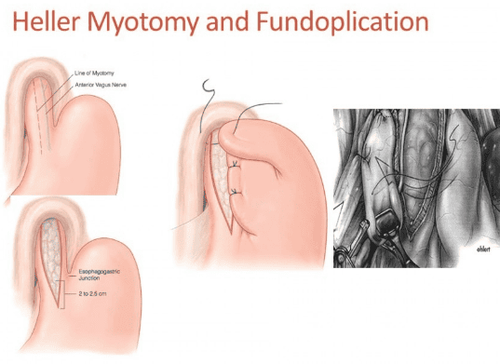
The standard surgical procedure for achalasia is laparoscopic Heller myotomy (LHM). This procedure creates a 3-cm myotomy through the lower esophageal sphincter over the anterior wall of the lower and upper esophagus of the stomach. This muscle ablation is performed in most patients with an aneurysm to reduce the risk of post-procedural reflux. Many long-term studies demonstrate the effectiveness of LHM in 85-90% of most patients.
4. Methods of treatment
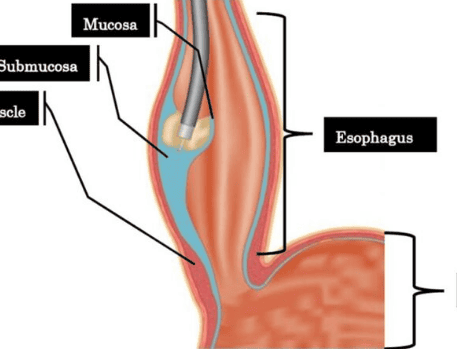
The newest endoscopic treatment for achalasia and related esophageal motility disorders is oral endoscopic endoscopic myomectomy (POEM). The four steps with POEM include: 1) incision of the mucosa of the esophageal wall; 2) make a submucosal tunnel to the upper part of the stomach; 3) cut the sphincter and/or longitudinal muscle from the distal esophagus to the upper stomach and 4) close the mucosal incision in the esophageal wall. Reports have demonstrated a reduction in dysphagia comparable to Heller myotomy but with a shorter recovery time, lower cost, and reduced cardiopulmonary complications. GERD is found to be more common after POEM procedures, however, because aneurysms are not performed after myomectomy. Randomized trials comparing POEM with Heller myotomy are underway.
5. Conclusion
Under normal circumstances, esophageal motility occurs in a coordinated, sequential manner to push food into the stomach. Esophageal motility disorders represent a diverse group of conditions that alter this motility in the esophageal or lower esophageal sphincter. The most common symptoms include difficulty swallowing and chest pain. Difficult to distinguish from other common diseases such as coronary artery disease, gastroesophageal reflux disease and malignancy. Standard work includes upper gastrointestinal endoscopy, barium esophagography, and high-resolution esophageal manometry. Treatment of achalasia focuses on reducing the pressure of the lower esophageal sphincter. Balloon dilation and laparoscopic Heller myotomy are the most commonly used treatments. Oral endoscopic myotomy (POEM) represents the newest endoscopic treatment option, and early data suggest comparable efficacy to Heller myotomy. As the diagnostic and therapeutic options for esophageal motility disorders are increasing, a multimodal approach is required and referral to gastroenterology or surgery is recommended for further management of these disorders.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
John Dewitt, update in the diagnosis and treatment of esophageal motility disorders, Dispatches from the guild conference, series
20, practicalgastro, march 2019 • volume XLIII, issue 3