This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Short bowel syndrome often occurs in people whose small intestine has been surgically removed in half or more, leaving the remaining length of intestine no more than 120cm, associated with poor absorption of nutrients .
1. Use of growth hormone in the treatment of short bowel syndrome
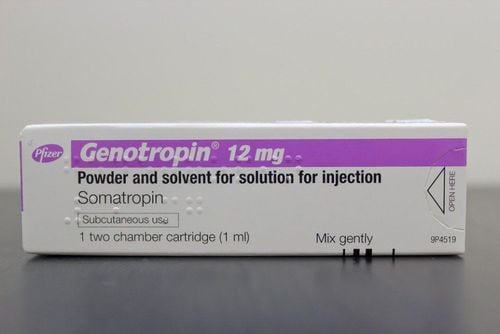
Growth hormone (somatropin, glutamine, Teduglutide) has been shown to promote crypt cell proliferation, stimulate mucosal growth, collagen deposition, and mesenchymal cell proliferation through insulin-like growth factor- 1 and an inhibitor of cytokine-2 signaling. Enhanced intestinal absorption has been repeatedly demonstrated in animal models of short bowel syndrome, whereas there are conflicting reports in humans.
In 1995, Byrne et al reported on 47 patients, most of whom had, treated with a combination of growth hormone, oral glutamine, and short bowel syndrome-optimized diet for 3 years. weeks in a controlled inpatient-like setting, followed by continued use of diet pills and glutamine. With a 5-year follow-up, they showed that 40% of patients were able to discontinue parenteral nutrition while another 50% could significantly reduce their use of parenteral nutrition. With these reports, the concept of intestinal rehabilitation was introduced.
2. A practical approach to stopping parenteral nutrition
Eligibility criteria used in phase III clinical trials provide only a guide to assist in determining which patients should be considered for factor nutrition. Currently, these agents should not be used in children outside the scope of clinical studies. Eligible patients include those with short bowel syndrome who neither have an obstructive nor inactive GI malignancy and are dependent on parenteral nutritional support or IVF despite optimized diet, oral fluids and adjuvants.
They must also be nutritionally optimized and fluid balance. Furthermore, the patient should be motivated with a desire to reduce or discontinue parenteral support. The presence/absence of colon and the length of the remaining small intestine are not necessarily determining factors in the selection of appropriate candidates and virtually any bowel anatomy can be considered.

3. What is important when stopping parenteral nutrition
Before stopping parenteral nutrition, regardless of the nutritional factor used, it is important for patients with short bowel syndrome to realize that it is important to stay away from parenteral nutrition to need more medications and increase daily food and liquid intake. Major lifestyle changes and increased out-of-pocket costs are often required. Therefore, patient education about the plan of care (eg, the diet and medications to be taken and the parenteral discontinuation plan) and ongoing support are important to enhance the outcome. compliance. This is best done in the context of multidisciplinary practice with healthcare providers experienced in the care of patients with short bowel syndrome.4. Caution when injecting somatropin or teduglutide drugs
Once daily subcutaneous injection is required to use somatropin or teduglutide. Because injection site reactions are relatively common, the injection site should be rotated between the abdomen, thighs, and upper arms. The injection should be given at the same time each day. Patients should be aware of the precautions required when using these medications and be instructed on how to appropriately monitor for complications and what to do/who to contact when problems occur. There are no data on the use of these agents in the presence of octreotide, biologic agents or immunosuppressive therapy.
Reduction of parenteral nutrition can be accomplished by reducing the number of days of parenteral nutrition per week or by reducing the amount of daily parenteral infusion equally throughout the week (eg, by 10% -30 %) .30 Patients tend to prefer the former; however, dehydration is of less concern. The teduglutide studies used the latter method while the phase III somatropin studies used the former.
5. Oral micronutrient supplementation when parenteral nutrition
Oral micronutrient supplementation becomes necessary once parenteral nutrition has been discontinued and levels should be periodically monitored. Electrolyte supplementation, usually magnesium and/or potassium and sometimes bicarbonate, may also be necessary and requires monitoring. The frequency of monitoring will depend on the stage at which parenteral nutrition is discontinued and the presence of existing or prior deficiencies. Routine laboratory follow-up will need to continue indefinitely, even in children who are completely discontinued from parenteral nutrition.

6. Conclusion
An important goal in the treatment of short bowel syndrome is to improve intestinal autonomy, thereby reducing and sometimes eliminating the need for parenteral nutritional support. After optimization of diet, hydration, and conventional pharmacological strategies (and sometimes surgical regenerative procedures), the use of nutritional factors has the potential to further reduce .
Currently available agents include somatropin, a recombinant human growth hormone, and teduglutide, a recombinant human GLP-2 analogue. Both agents, although quite different in duration, cost, and adverse events, have been shown in randomized, placebo-controlled trials to facilitate cessation of parenteral nutrition. . Long-term safety and efficacy, short duration of dosing associated with bowel syndrome onset, optimal patient selection to use, duration of treatment, and cost-effectiveness of both the somatropin and teduglutide strategies would require be studied further.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Messing B, Crenn P, Beau P, et al. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 1999;117:1043-1050. Amiot A, Messing B, Corcos O, et al. Determinants of home parenteral nutrition dependency and survival of 268 patients with non-malignant short bowel syndrome. Clin Nutr 2013;32:368-74. Byrne TA, Persinger RL, Young LS, et al. A new treatment for patients with short-bowel syndrome: growth hormone, glutamine, and a modified diet. Ann Surg 1995;222:243-254. Byrne TA, Cox S, Karimbakas M, et al. Bowel rehabilitation: an alternative to long-term parenteral nutrition and intestinal transplantation for some patients with short bowel syndrome. Transplant Proc 2002;34:887-890.