This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Successful treatment of patients with Short Bowel Syndrome (SBS) depends on residual intestinal adaptation, requiring a combination of pharmacological and nutritional therapy. Although the short bowel syndrome diet is quite similar for people with and without colonic segments, some key differences should be noted. This article focuses on dietary interventions that enhance adaptation, increase absorption and, as a result, reduce stool volume.
1. Overview
Without active use of pharmacological agents, diet alone is generally not effective in limiting severe diarrhea in patients with short bowel syndrome. However, dietary therapy is an important component of care in these patients. The cornerstone of dietary therapy is the adjustment of food intake to facilitate maximum nutrient and fluid use by reducing stool volume. Stool output in short bowel syndrome is driven by fluid loads that exceed the absorptive capacity of the shortened intestine; but other factors also contribute.
For example, in addition to the loss of absorptive surface area, feedback mechanisms controlling acid and bicarbonate transport and secretion are often impaired. A clear understanding of these factors is essential for selecting the best therapeutic interventions.
2. Initial nutritional assessment
The initial evaluation of all patients with short bowel syndrome should include a comprehensive nutritional assessment. Information obtained should include a history of weight change, medication use (including complementary and over-the-counter medications), the presence of other symptoms that may affect fluid intake or loss, potential signs/symptoms of micronutrient deficiency and physical assessment for signs of dehydration and malnutrition.
Additional information that should be collected at baseline includes relevant past medical, psychiatric and surgical history, including comorbidities and the presence of bowel complications such as tube mouth splicing; chronic congestion; percutaneous fistula; and peritoneal drainage. A history of nutritional support should also be obtained, including information regarding enteral and/or central venous access devices, formulation used, route and method of administration, and complications. known before. Finally, given the high level of motivation required to adhere to prescribed diets, fluids, and medical treatments, it is helpful to inquire about education, motivation, system their support and potential economic or other barriers.
3. Control the amount of fluid in and out of the body
Patients with short bowel syndrome should be instructed on how to measure daily fluid intake and urine/faeces, as periodic assessment of these parameters helps direct fluid requirements. It is also helpful to review a food diary, preferably over a period of several days, to determine the typical short bowel syndrome patient's diet and daily energy intake. A baseline assessment of electrolytes and micronutrient levels (see micronutrients section below) should be performed at the initial examination. Because of the high risk of metabolic bone disease in these patients, bone density should be assessed initially and followed up every 1–2 years.
4. Diet - Lessons Learned
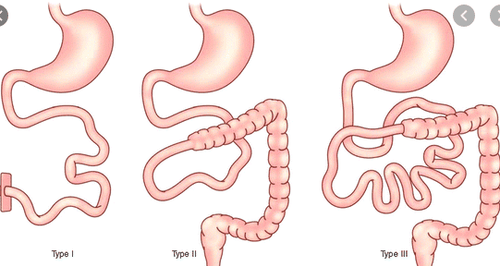
Initial evidence supporting a beneficial effect of dietary therapy in patients with short bowel syndrome is based on a limited number of studies including a small number of patients with different bowel anatomy. These studies typically demonstrate a decrease in stool volume and an increase in absorption depending on the remaining bowel anatomy and the type and amount of carbohydrates and fats used. In particular, patients with short bowel syndrome with a remaining segment of the colon seem to derive the most benefit in terms of nutrient absorption and reduced stool loss from a diet high in complex carbohydrates, low in moderate fat, and low in fat. right. In an inpatient setting, Byrne et al followed nearly 400 patients over a 10-year period following intensive counseling and close follow-up for 2-4 weeks and further demonstrated the importance of diet. short bowel syndrome for the improvement of stool volume and both nutritional and hydration status. They concluded that colonic patients benefited from a different diet than those without colons.
Patients with a terminal jejunostomy usually absorb more nutrients than fluids, so they may need at least intravenous (IV) fluids initially. In contrast, in patients with short bowel syndrome with an jejunostomy or ileostomy, more sodium and water are absorbed, and these patients may require more nutrients than fluids. For all patients with short bowel syndrome, the most important dietary interventions are to feed less frequently, to avoid simple sugars in any form, and to chew food thoroughly. The long-term success of the optimal short bowel syndrome diet requires intensive education, counseling, and adequate nutritional supervision to maintain compliance and achieve intestinal resilience. independence of parenteral nutrition and intestinal autonomy. One of the key roles of a dietitian is to translate all the data into foods and meals that meet an individual's preferences and lifestyle. Patients not only need to be informed about what they need to avoid but more importantly what they can eat.

5. Absorption capacity in patients with short bowel syndrome
In general, most stable adult short bowel syndrome patients absorb only about one-half to two-thirds of normal energy; therefore, dietary intake must be increased by at least 50% of their estimated needs (ie, a “hyperphagic” diet). However, in some people, this increased intake may contribute to excessive loss of micronutrients and fluids from worsening diarrhea. Setting daily calorie and fluid intake goals is achieved by careful monitoring. May require adjustment based on tolerability, as determined by symptoms, stool volume, ongoing assessment of what they eat, and in doing so, assessment of the patient's understanding of dietary therapy , along with micronutrient levels, changes in weight, and hydration status.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














