This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalProton Transfer Reaction-Mass Spectrometry is a method of using breath to check patients for esophageal cancer.
1. Urgent biomarkers of esophageal cancer
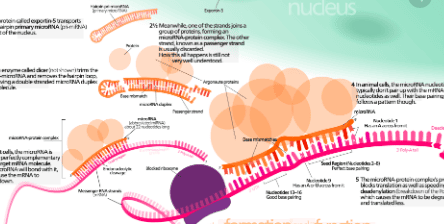
1.1 Blood biomarkers Autoantibodies have attracted interest as serological markers for esophageal cancer, due to their stability and persistence in serum samples. With improvements in antibody detection technology raising the detection limit, there is increasing interest in the utility of autoantibodies as diagnostic and prognostic biomarkers for esophageal cancer. Perhaps the most comprehensively studied is the tumor suppressor gene, TP53. The protein product of TP53 is a nuclear phosphoprotein and in normal human plasma, TP53 protein and anti-p53 antibodies are absent.1.2 The role of miRNA strand miRNA is a single-stranded, non-coding RNA that can regulate the expression of genes and proteins. miRNAs are highly expressed in a stable form, with high levels of inter-individual consistency in a variety of extracellular fluids including serum and plasma, and have attracted attention as biomarkers for cancer. mail and illness. Recent studies have reported circulating plasma/serum miRNAs as potential diagnostic and prognostic markers in several gastrointestinal cancers - esophageal squamous cell carcinoma, esophageal adenocarcinoma, stomach and colon. Although still an emerging area of research, recent meta-analyses have highlighted the potential of circulating miRNAs in the detection of esophageal cancer.
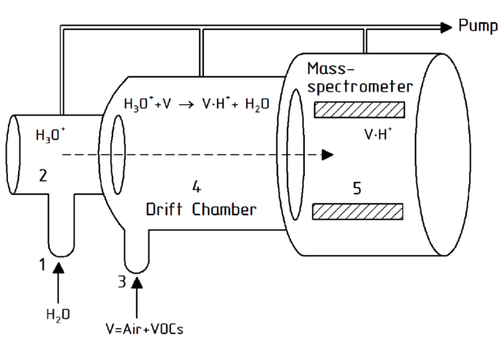
Many studies have shown that breath alkanes are associated with cancer, perhaps as a biological product of the oxidative stress pathway. Breath ethane was previously studied in end-stage esophageal squamous cell carcinoma and adenocarcinoma, with no difference from healthy controls. More advanced technologies have been used to characterize VOCs associated with esophageal cancer. Headspace analysis of urine and gastric contents from esophageal cancer patients using selected ion-flow tube mass spectrometry identified a number of VOCs that were differentially regulated compared with healthy controls. However, there is no dominant group of VOCs in the cancer group.

In addition, the authors found that the VOC profile distinguishes esophageal cancer from Barrett's metaplasia and from benign conditions of the upper gastrointestinal tract (including esophagitis, esophageal stricture, and esophageal candidiasis). ). Developing a risk prediction model, the authors reported eight important predictors for adenocarcinoma: decanal, nonanal, phenol, ethyl phenol, methyl phenol, hexanoic acid, heptanal and butyric acid, with a sensitivity and specificity of 98% and 91.7%, respectively, when compared with the normal upper gastrointestinal tract. Furthermore, the model correctly distinguished esophageal adenocarcinoma from noncancerous controls (benign condition, Barrett metaplasia, and normal upper gastrointestinal tract), with sensitivity and specificity. are 87.5% and 82.9%, respectively. Interestingly, no difference in VOCs was detected between early- and late-stage cancers, or between tumor size and VOCs concentrations.
1.5 The role of mass spectrometry-proton transfer reaction – a new breath test method for the diagnosis of esophageal cancer

2. Conclusion
The recently developed field of breath and gas analysis for cancer detection represents a completely non-invasive approach to early detection and continuous screening of those at risk. With improvements in the sensitivity of VOC detection technology, it is likely that the pool of breath and odor biomarkers will increase significantly. Although there are relatively few studies investigating breath biomarkers in esophageal cancer, early predictive models have shown some promise. Moving forward in this rapidly growing field, it is important to use standard approaches to breath sample collection, to minimize research heterogeneity. Furthermore, there is little evidence to support the biological origin of VOCs.As the incidence of esophageal cancer continues to increase worldwide, new diagnostic and prognostic tools are needed to improve survival and direct clinical management. Advances being made in new minimal and non-invasive biomarkers represent a suite of ancillary tests that can stratify patients for endoscopy and other imaging modalities, ultimately leading to to improve patient care. While it is unlikely that there will be a single “silver bullet” biomarker, the most likely scenario would be derived from prediction algorithms based on multiple biomarkers, which may also include combined blood and breath analysis.
Currently, screening for gastrointestinal cancer is a scientific and effective measure for early detection of gastrointestinal cancer (esophageal cancer, stomach cancer, colon cancer) and giving a treatment plan. best treatment. Currently, Vinmec International General Hospital has a package of screening and early detection of cancers of the gastrointestinal tract (esophagus - stomach - colon) combined with clinical and paraclinical examination to bring the most accurate results. maybe.
When screening for gastrointestinal cancer at Vinmec, you will receive:
Gastrointestinal specialty examination with an oncologist (by appointment). Gastroscopy and colonoscopy with an NBI endoscope with anesthesia. Peripheral blood count (laser counter). Automated prothrombin time test. Automated thrombin time test. Activated Partial Thromboplastin Time (APTT) test using an automated machine. General abdominal ultrasound
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References1. Pakzad R , Mohammadian-Hafshejani A, Khosravi B, Soltani S, Pakzad I, Mohammadian M, Salehiniya H, Momenimovahed Z. The incidence and mortality of esophageal cancer and their relationship to development in Asia. Ann Transl Med. 2016; 4:29. [PubMed] [DOI]
2. Bystricky B , Okines AF, Cunningham D. Optimal therapeutic strategies for resectable oesophageal or oesophagogastric junction cancer. Drugs. 2011; 71 :541-555. [PubMed] [DOI]
3. Bandla S, Pennathur A, Luketich JD, Beer DG, Lin L, Bass AJ, Godfrey TE, Little VR. Comparative genomics of esophageal adenocarcinoma and squamous cell carcinoma. Ann Thorac Surg. 2012; 93 :101-1106. [PubMed] [DOI]
4. Bird-Lieberman EL, Fitzgerald RC. Early diagnosis of oesophageal cancer. Br J Cancer. 2009; 101 :1-6. [PubMed] [DOI]
5. Yentz S, Wang TD. Molecular imaging for guiding oncologic prognosis and therapy in esophageal adenocarcinoma. Hosp Pract (1995). 2011; 39 :97-106. [PubMed] [DOI]
6. Jankowski J , Barr H, Wang K, Delaney B. Diagnosis and management of Barrett's oesophagus. BMJ. 2010; 341 :c4551. [PubMed] [DOI]
7. Roger Yazbeck, Simone E Jaenisch, David I Watson. From blood to breath: New horizons for esophageal cancer biomarkers, World J Gastroenterol. Dec 14, 2016; 22(46): 10077-10083.