This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalEsophageal cancer is a potentially fatal cancer that includes the subtypes of adenocarcinoma and squamous cell carcinoma. Worldwide, the incidence of esophageal cancer is increasing rapidly, associated with an increase in the incidence of related risk factors. Early diagnosis of esophageal cancer will increase the effectiveness of treatment and prolong the patient's survival time.
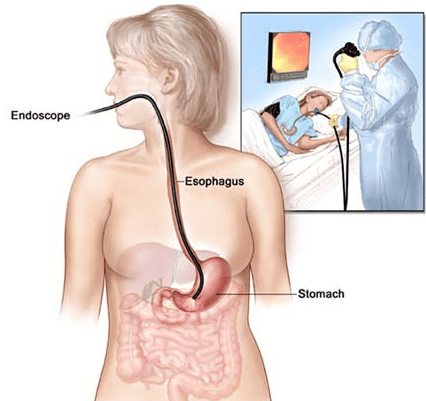
The asymptomatic nature of esophageal cancer often leads to a late diagnosis and a five-year survival rate of less than 15%. Current diagnostic tools are limited, including only invasive procedures such as gastrointestinal endoscopy, biopsy, and histopathology. In fact, minimal and noninvasive biomarkers of esophageal cancer are needed to facilitate earlier detection and better clinical management of patients. The following article summarizes the developments and clinical implications of esophageal cancer biomarkers, focusing on circulating markers, and the new field of breath and biomarkers. smelly.
1. Esophageal Cancer Overview
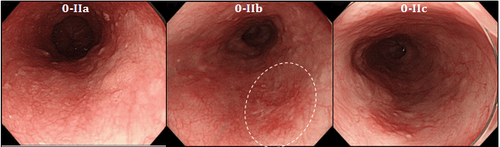
Esophageal cancer is the sixth leading cause of cancer death worldwide. Histologically, it is classified into 2 subtypes, squamous cell carcinoma and adenocarcinoma, each with a specific cellular origin, pathogenesis, and epidemiology.The current gold standard techniques for detecting and diagnosing esophageal cancer are endoscopic and biopsy is invasive. Furthermore, due to the absence of symptoms at an earlier stage of the disease, presentation and diagnosis are often late, resulting in a poor prognosis and 5-year survival rates as low as 15%. Early diagnosis is associated with a much higher 5-year survival rate, and when limited to mucosal disease, specific survival rates of up to 98% have been reported. Better diagnostic methods are needed to move the majority of diagnoses to the earliest stages, and the expansion of access to routine endoscopy and wider use in the context of screening is not clinically effective. cost. Minimal and noninvasive biomarkers, mainly in blood and breath, represent the most likely candidates to facilitate early detection of esophageal cancer.
The pathogenesis of squamous cell carcinoma is complex, involving the accumulation of genetic alterations in the esophageal mucosa, causing progressive changes leading to invasive carcinoma. Environmental factors, diet, smoking and alcohol consumption are closely related to the molecular mechanism of squamous cell carcinoma; however, evidence of a cause-and-effect relationship is lacking. Inherited mutations within cyclin D1 and the tumor suppressor gene, TP53, are among the most frequently isolated genetic abnormalities from esophageal squamous cell carcinoma.
TP53 is a tumor suppressor gene that plays a role in DNA repair and cell cycle arrest, and is the most common mutation found in cancers, including squamous cell carcinoma. Esophageal. TP53 mutations have been reported in at least 10% and up to 80% of esophageal squamous cell carcinomas. In addition, mutations for the TP53 gene were also found in dysplastic lesions, suggesting that TP53 mutations may be an event in the early stages of esophageal squamous cell carcinoma. The mutant TP53 produces abnormal TP53 protein that accumulates in the cell nucleus that can be identified by immunohistochemistry.
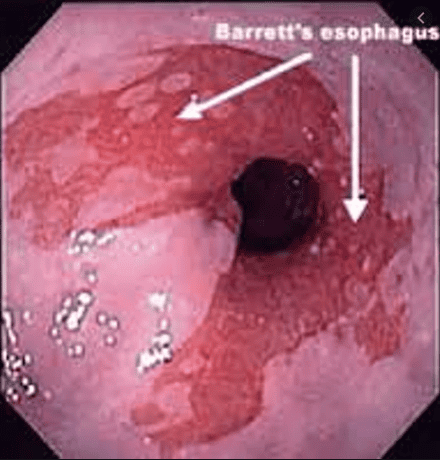
1.3 Esophageal adenocarcinoma Esophageal adenocarcinoma is a potentially fatal tumor that usually develops in the lower third of the esophagus, or at the gastro-oesophageal junction. Incidence has gradually increased in developed countries since 1984, with a 4% increase in the incidence of adenocarcinoma in Australia between 1988 and 2005. Adenocarcinoma is most common in men, the elderly and the obese. However, the most important risk factor identified for adenocarcinoma is Barrett's esophagus.
Barrett's esophagus is a metaplasia of the esophageal epithelium, affecting 2% of the adult population. It is confirmed histologically by replacing normal stratified squamous epithelium with columnar epithelium with intestinal metaplasia as determined by the presence of goblet cells due to chronic gastroesophageal reflux disease. count. Patients with Barrett's esophagus are at increased risk for progression to adenocarcinoma, with some studies showing that 40%-75% of adenocarcinoma cases have no evidence of arrett's esophagus. . It is thought that the absence of any evidence of Barrett's esophagus may indicate an alternative, as-yet-unidentified pathogenesis, and Barrett's esophagus is simply a strong risk factor in a small subset. population, but not a necessary carcinogen. progression of esophageal adenocarcinoma. However, the absence of useful tools for early identification and ongoing evaluation of Barrett's esophagus and progression to adenocarcinoma has made assessing this relationship difficult.
2. Urgent biomarkers of esophageal cancer
2.1 Blood biomarkers Autoantibodies have attracted interest as serological markers for esophageal cancer, due to their stability and persistence in serum samples. With improvements in antibody detection technology raising the detection limit, there is increasing interest in the use of autoantibodies as diagnostic and prognostic biomarkers for esophageal cancer. Perhaps the most comprehensively studied is the tumor suppressor gene, TP53. The protein product of TP53 is a nuclear phosphoprotein and in normal human plasma, TP53 protein and anti-p53 antibodies are absent. The p53 mutation can cause the accumulation of non-functional proteins with increased stability and longer half-lives compared with native proteins. Anti-p53 production has subsequently been detected in the tissues, blood, and other body fluids of several types of cancer, including esophageal cancer.Circulatory tumor cells (CTCs) are derived from the primary tumor, and are released into the systemic circulation, where they can form micro-metastases. Various tests have been developed and used to assess the diagnostic and prognostic capabilities of CTCs in several types of cancer, including breast, colorectal, gastric, and esophageal cancers. A recent meta-analysis by Qiao et al aimed to determine the association between CTCs with clinical and prognostic features (tumor stage, lymph node metastasis, distant metastasis, and survival time of CTCs). patients) in esophageal cancer. New methodologies for the quantification of circulating tumor DNA may also offer new diagnostic potential, but further research is needed to evaluate this possibility.
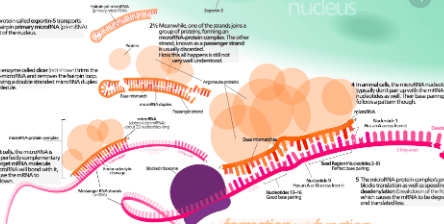
2.2 Role of miRNA strand miRNA is a single-stranded, non-coding RNA that can regulate the expression of genes and proteins, miRNAs are highly expressed in stable form, with a high degree of consistency between individuals over many Extracellular fluids include serum and plasma, and have attracted attention as biomarkers for cancer and disease.
2.4 Breath test - a new means of diagnosing esophageal cancer The first breath analysis study to determine breath VOCs in esophageal cancer identified a dominant expression pattern of phenol, with phenol, methyl phenol, ethyl phenol and hexanoic acid were significantly increased in esophageal cancer compared with healthy controls. In the most comprehensive study to date, Kumar et al investigated breath VOCs in esophageal squamous cell carcinoma, esophageal adenocarcinoma, Barrett's esophagus, and benign and cancerous conditions. gastric adenocarcinoma, compared with healthy controls. A total of 12 VOCs, including phenols, aldehydes, and fatty acids were identified as discriminating against esophageal cancer and gastric cancer compared with normal upper gastrointestinal (GI) tract

3. Conclusion
Current diagnostic and monitoring procedures for esophageal cancer are invasive, costly, and inadequate for early detection. Recent advances have been made in the development and validation of novel minimal and non-invasive biomarkers for esophageal cancer. Although several new serological markers have been investigated, they have not yet been translated into use as tools in clinical practice. Circulating antip53 and CTCs have shown the most promise as diagnostic and prognostic markers of esophageal cancer, with recent meta-analyses supporting their use.Gastrointestinal cancer screening is a scientific and effective measure for early detection of gastrointestinal cancers (esophageal cancer, stomach cancer, colon cancer) and providing a good treatment plan. best. Currently, Vinmec International General Hospital has a package of screening and early detection of cancers of the gastrointestinal tract (esophagus - stomach - colon) combined with clinical and paraclinical examination to bring the most accurate results. maybe.
When screening for gastrointestinal cancer at Vinmec, you will receive:
Gastrointestinal specialty examination with an oncologist (by appointment). Gastroscopy and colonoscopy with an NBI endoscope with anesthesia. Peripheral blood count (laser counter). Automated prothrombin time test. Automated thrombin time test. Activated Partial Thromboplastin Time (APTT) test using an automated machine. General abdominal ultrasound
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References1. Pakzad R , Mohammadian-Hafshejani A, Khosravi B, Soltani S, Pakzad I, Mohammadian M, Salehiniya H, Momenimovahed Z. The incidence and mortality of esophageal cancer and their relationship to development in Asia. Ann Transl Med . 2016; 4:29. [PubMed] [DOI]
2. Bystricky B , Okines AF, Cunningham D. Optimal therapeutic strategies for resectable oesophageal or oesophagogastric junction cancer. Drugs . 2011; 71 :541-555. [PubMed] [DOI]
3. Bandla S, Pennathur A, Luketich JD, Beer DG, Lin L, Bass AJ, Godfrey TE, Little VR. Comparative genomics of esophageal adenocarcinoma and squamous cell carcinoma. Ann Thorac Surg . 2012; 93 :101-1106. [PubMed] [DOI]
4. Bird-Lieberman EL, Fitzgerald RC. Early diagnosis of oesophageal cancer. Br J Cancer . 2009; 101 :1-6. [PubMed] [DOI]
5. Yentz S, Wang TD. Molecular imaging for guiding oncologic prognosis and therapy in esophageal adenocarcinoma. Hosp Pract (1995). 2011; 39 :97-106. [PubMed] [DOI]
6. Jankowski J , Barr H, Wang K, Delaney B. Diagnosis and management of Barrett's oesophagus. BMJ . 2010; 341 :c4551. [PubMed] [DOI]
7. Roger Yazbeck, Simone E Jaenisch, David I Watson. From blood to breath: New horizons for esophageal cancer biomarkers, World J Gastroenterol. Dec 14, 2016; 22(46): 10077-10083.