This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalOver the past 4 decades, the problem of researching Helicobacter pylori (H. pylori) bacteria has occupied the minds of many scientists around the world. H. pylori is a bacteria commonly found in patients with chronic gastritis, peptic ulcer disease, and stomach cancer as well as in healthy individuals.
H. pylori was first reported in 1875, when Bottcher and Letulle observed it at the margins of peptic ulcers. Although the prevalence of this organism was later proven, its discovery occurred only in the early 1980s. It is clear that since 1983 H. pylori has colonized more than half of the population. world. This event generated a great multidisciplinary interest including gastroenterologists, microbiologists and infectious disease specialists among others.
1. The role of H. pylori as a true pathogen has been at the center of great discussion for many years.
H. pylori infection is associated with gastric and duodenal ulcers (in 1%-10% of infected patients), gastric carcinoma (0.1%-3%), and mucosal connective tissue lymphomas gastric mucosa (MALT) (less than 0.01%.). However, the majority of the infected population will never develop symptoms associated with H. pylori infection. H. pylori enters the human stomach appearing early in life and persists indefinitely unless treated. At the same time, the transmission of H. pylori is mainly in the home environment. The decrease in H. pylori prevalence over time was first reported in 1997, and subsequently confirmed in two large population-based studies in the United States. Due to the gradual decline of H. pylori, a variety of negative consequences have been described. There has been an alarming increase in asthma, as well as an increased likelihood of diarrheal illnesses. However, a more serious consequence associated with the decline of H. pylori is an increase in esophageal diseases, such as gastroesophageal reflux disease (GERD), Barrett's esophagus, and carcinoma. glandular tissue of the esophagus. We do not know whether the decline in the number of H. pylori infections is the cause of these emerging diseases or if it is just an indicator of the hygiene hypothesis. Due to its low virulence and the fact that the disease is observed mostly in infected elderly individuals, H. pylori can be considered as a cohabitant and only as an opportunistic pathogen.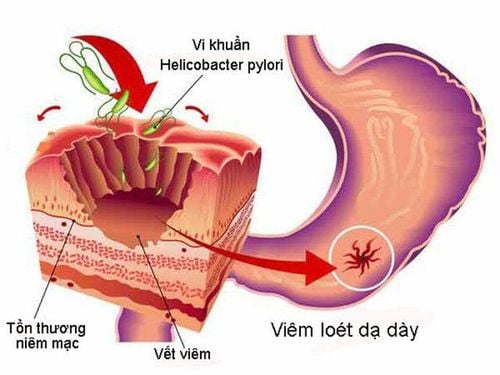
2. Diseases associated with H. pylori
Available data may suggest that H. pylori persistence in the stomach is involved in the development of gastrointestinal diseases, such as chronic gastritis, peptic ulcer disease, and carcinoma. gastric glandular tissue and gastric MALT lymphoma. Recent data suggest a statistically significant relationship between H. pylori detection and pancreatic cancer development.Factors for the development of gastrointestinal symptoms with H. pylori infection The risk of developing gastrointestinal symptoms depends on the degree of pathogenicity of a persistent strain, the genetic characteristics of the host , environmental factors and dietary patterns. The researchers emphasize the fact that the persistence of H. pylori in the gastric mucosa is constantly controlled by the immune system, hence the pathogenic properties of H. pylori and, therefore, the symptoms. of the disease manifests itself in the presence of favorable factors. Beyond that time, more and more people are paying attention to the implication of H. pylori in the pathogenesis of extragastric diseases. Therefore, the role of microorganisms in the development of a number of neurological, cardiovascular, hematological, dermatological and metabolic diseases is under active investigation. The results of the available studies are certainly quite contradictory and require a more thorough study. The meta-analysis by Wang et al demonstrated that chronic H. pylori infection is a predictor for the development of ischemic brain injury. Reports showing a relationship between the detection of H. pylori and the development of Alzheimer's disease have been published. Huang et al were able to establish that the risk of Parkinson's disease was significantly higher in the H. pylori-positive group than in the H. pylori-negative (HPN) group (adjusted hazard ratio: CI 2.29.95). %: 1.44–3.66; P < 0.001). Substantial relationship between H. pylori detection and cardiovascular disease Limited experience has been accumulated in studying the influence of H. pylori on the development of cardiovascular diseases. Several studies confirm a significant relationship between the detection of H. pylori, the development of atherosclerotic vascular lesions, and the consequent higher risk of coronary heart disease. Jukic et al found that H. pylori-positive patients were more likely to have hypertension (P = 0.014), higher systolic blood pressure (P = 0.043) and diastolic blood pressure (P = 0.005), as well as increased plasma triglyceride concentrations (P=0.013) and low antisecretory high-density lipoprotein levels (P=0.01). At the same time, there was no significant difference in disease severity between the two groups.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References Reshetnyak VI, Burmistrov AI, Maev IV. Helicobacter pylori : Commensal, symbiont or pathogen? . World J Gastroenterol 2021; 27(7): 545-560 [PMID: 33642828 DOI: 10.3748/wjg.v27.i7.545]