This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
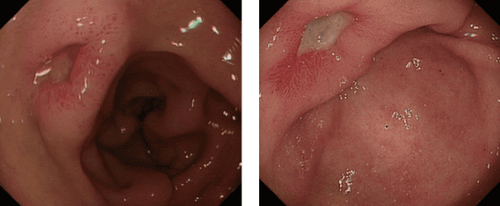
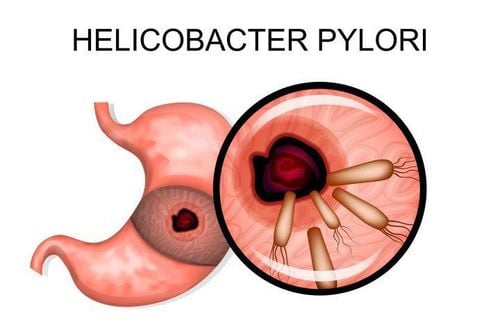
Helicobacter pylori (H. pylori) is an important cause of peptic ulcer disease and gastric malignancies. The treatment of H. pylori remains a challenge, because many factors determine the success of therapy such as resistance to primary or secondary antibiotics, drug concentrations on the mucosa, patient compliance, side effects and costs.
1. Current status of HP treatment
While no new drugs have been developed, current therapy is still based on different mixtures of known antibiotics and antacids. A standard triple therapy consisting of two antibiotics and a proton pump inhibitor is suggested as the first line regimen. Bisthmuth-containing quadruple therapy, sequential or quadruple bisthmuth-free therapy (concurrently) is also an alternative therapy. Levofloxacin containing a regimen I of a triple drug is recommended as a life-saving treatment for H. pylori infection after failure of first-line therapy. Antibiotic resistance rapidly reduces the effectiveness of any regimen associated with these remedies. Therefore, the addition of probiotics to the drug, the development of anti-H.Pylori drugs by photodynamic therapies, and the successful achievement of an H. pylori vaccine may hold promise for synergistic or synergistic results against H. pylori, because each has different effects.

The Maastricht IV/Florence consensus report recommended bismuth-containing quadruple therapy as an alternative to first-line empiric therapy in areas with clarithromycin resistance greater than 15%-20%. If this regimen is not available sequential therapy or quadruple non-bismuth therapy (the so-called “concurrent” treatment) is recommended. After treatment for PPI-clarithromycin-containing H. pylori infection has failed, bismuth-containing quadruple therapy or levofloxacin-based triple therapy is recommended as second-line or salvage therapy.
The Maastricht IV/Florence Consensus Report recommended the use of antibiotic susceptibility testing (culture-guided therapy), after failure of second-line therapy. However, culture-guided third-line therapy has been recommended, but if antibiotic sensitivity data are not available, empiric triple or quadruple therapy may be recommended as regimen. third line.
2. Antibacterial agents and the problem of antibiotic resistance
Despite the number of studies, the optimal treatment for H. pylori infection has not been established and the usual clinical treatments are usually triple or quadruple antibiotic therapy.
Prevalence of antibiotic resistance to antibiotics varies in different geographical regions and is related to antibiotic consumption in those regions. The most commonly used antibiotics are imidazole (metronidazole or tinidazol), macrolides (clarithromycin or azithromycin), tetracycline, amoxicillin, rifabutin, and furazolidone. Bismuth, an anti-Hpylori agent, is used in bismuth-based quadruple therapy and appears to almost completely maintain a high eradication rate, independent of the problem of antibiotic resistance.
A large body of evidence indicates that in order to identify an appropriate antibiotic in drug regimens against H. pylori infection, information on antibiotic susceptibility of this bacterium in different geographical areas is required. In the world.
2.1. Anti-acids PPI
Treatment of H. pylori involves a combination of antibacterial agents (antibiotics) and anti-acids (PPIs) for 7 to 14 days. PPIs inhibit parietal cells H + / K + adenosine triphosphatase (ATPase), the enzyme of the tubular membrane of gastric parietal cells responsible for the final step in gastric acid secretion. Inhibition of this enzyme is more effective than H2-receptor antagonists in inhibiting gastric acid secretion.
At low pH, the PPI in the stomach as an acid-activated prodrug converts to the spiro-intermediate of dihydrobenzimidazole, which then undergoes aromaticization to sulfenic acid, which is then dehydrated to form a quaternary sulfonamide ring. PPIs bind to various cysteines in the α subunit of H+/K+ ATPase and inhibit the enzyme.
PPIs with anti-secretory effects reduce acid production from the stomach, allowing tissues damaged by infection to heal. PPIs can also make acid-labile antibiotics more stable as gastric pH increases, and can also alter antibiotic concentrations by transporting antibiotics from plasma into gastric juice and improving successful eradication rate.
2.2. Treatment regimens
Dual therapy (2-drug regimen)
Dual therapy including PPIs with clarithromycin or amoxicillin or metronidazole has been popular in previous decades. Dual therapy is now obsolete due to the ineffectiveness of clarithromycin and metronidazole. In contrast, amoxicillin resistance of primary and secondary H. pylori worldwide is generally low and rare, although it is a common agent in standard triple therapy and is therefore suitable for use. used in the dual treatment of H. pylori infection.
Amoxicillin is effective at high pH (> 5.5). According to some controversial data, PPIs at standard doses would not be able in rapidly metabolisers to achieve sufficient pH to inhibit effective antibiotic activity in gastric mucus, determining lower eradication rates. after treatment with a standard-dose PPI-containing regimen.
Triple therapy
H. pylori triple therapy consisting of PPIs, amoxicillin and clarithromycin is used as first-line therapy. Resistance to clarithromycin or metronidazole is associated with reduced success rates, an important cause of H. pylori treatment failure. Other factors such as rapid metabolism of PPIs by CYP2C19, poor patient adherence, high gastric acidity and bacterial load appear to be the main causes of H.Pylori eradication failure.
One hundred and thirty-six patients enrolled in the study for 3-day 10-time therapy consisting of esomeprazole plus amoxicillin and metronidazole. The cure rate of patients was 82.4% according to ITT analysis and 88.2% according to PP analysis. Based on several existing clinical trials, it seems likely that quinolone-based triple therapy would be effective as first-line therapy in H. pylori infection. The use of levofloxacin as an alternative to clarithromycin in triple therapy and sequential therapy was studied by Qian et al. 7-d triple therapy of levofloxacin (levofloxacin, amoxicillin, esomeprazole) produced no therapeutic effect. satisfactory results, only sequential therapy containing levofloxacin achieved a satisfactory outcome.
Quadruple regimen
Quadruple therapy including bismuth subcitrate, PPIs, metronidazole and tetracycline has been better accepted than standard triple therapy in some studies. Four-day therapy containing bismuthate dicitrate, esomeprazole, levofloxacin, and tetracycline showed a success rate of 95.8% after failure of sequential therapy. This regimen may be used as a good option in areas of high clarithromycin resistance. In a similar study, 14-day therapy with esomeprazole, amoxicillin, levofloxacin, and bismuth achieved elimination rates of more than 90% after failure of concomitant or serial therapy.
Serial therapy
An Italian innovation in quadruple therapy resulted in serial therapy consisting of dual therapy for 5 days with amoxicillin and PPIs and an additional 5 days with tinidazole, clarithromycin and PPIs. This regimen was studied in 52 patients with H. pylori infection and an eradication rate of about 98% was achieved with ITT analysis. Another study evaluating the success rate of sequential therapy compared with standard triple therapy found that 10-day sequential therapy was better than standard triple therapy in children, which is confirmed by studies performed in adults.
3. Future prospects in the treatment of H.pylori
The overuse of antibiotics and the accumulation of point mutations in the DNA of H. pylori are considered to be the main causes of increasing antibiotic resistance. Currently, the recommendation of two weeks of antibiotics or high-dose PPIs is often associated with the development of undesirable side effects and patient complaints during anti-H. pylori therapy.
A large number of H. pylori eradication reports from different geographic areas show conflicting results, and one treatment regimen can be extremely effective in one geographic area and yield results. Unsatisfactory results in other regions. In 2010, an H. pylori strain isolated from a 31-year-old woman with gastric cancer was resistant to all seven of the antibiotics tested: clarithromycin, metronidazole, amoxicillin, tetracycline, furazolidone, erythromycin, and ciprofloxacin. . The search for new molecules to treat H. pylori infection is part of ongoing research programs.
Therefore, the development of a new and alternative treatment regimen for eradicating H. pylori while reducing the frequency of adverse events would be an invaluable advance.
3.1. Probiotics
Probiotics, live microorganisms mostly belonging to the genus Lactobacillus, Bifido bacteria and the genus Saccharomyces, when used in sufficient quantities, will provide health benefits to the host beyond the inherent basic nutrition.
Current interest in the efficacy of probiotics against H. pylori and its activity in reducing bacterial colonization and reducing gastritis has been stimulated because it offers a routine alternative. large tissue and low cost to prevent or reduce H. pylori colonization.
However, conflicting data have been obtained with probiotics treatment. The addition of yogurt to PPI-based triple therapy improved cure rates but adverse events were the same as in the control group with standard triple therapy.
Efficacy of probiotic supplementation on H. pylori eradication and adverse events conducted in May 2014 showed that specific probiotic strains could improve H. pylori eradication rates , especially when antibiotic therapies are relatively ineffective. This meta-analysis observed no significant reduction in adverse events therefore, notable heterogeneity was observed with respect to the overall occurrence of adverse events.
The use of probiotics as an adjuvant therapy, which seems promising for the current eradication of H. pylori, aims to reduce the frequency of antibiotic-induced adverse events, although still needed. must be optimized.
3.2. Herbal Compound
In recent years, several studies have suggested that phytomedicine has an additional function in the treatment of H. pylori, and can prevent H. pylori infection through the use of cheap, safe and non-invasive anti-H. toxic. pylori formula from medicinal plants.
Regarding the ability of plant extracts to reduce antibiotic resistance, the anti-mutagenic properties of some plant extracts on the rate of mutations leading to clarithromycin resistance in H. pylori were evaluated. The results of this study show the remarkable effectiveness of Mirtus communis extract, Teucrium polium in preventing antibiotic resistance. This could be more beneficial if medicinal plants combined with current antibiotic regimens are used to develop more effective eradication regimens. However, the mode of action, cytotoxic potential, and benefits of herbal medicine are complex, incomplete, and confusing. Further evaluation of the pharmacokinetics of such products in animals and the design of precise clinical trials of promising herbal products should be addressed in future investigations.
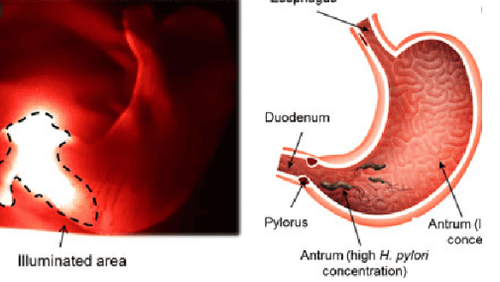
3.3. Photodynamic therapy
Microbial photoactive inactivation is based on a combination of dyes called sensitizers or sensitizers and innocuous visible light of suitable wavelength to produce a triplet excited state ( 3O2) of the dye molecules, in turn, can react with molecular oxygen resulting in the production of various cytotoxic reactive oxygen species such as superoxide-anion radicals (O2 • -) and single molecular oxygen (1O2). Recently, several in vitro and in vivo studies to develop anti-H.pylori Photodynamic Therapy for H. pylori eradication have been successful.
H. pylori is sensitive to blue light inactivation, which may represent a new therapeutic approach, especially in patients who have failed standard antibiotic therapy. Blue light irradiation produced a rapid decrease in the number of bacteria in the blue light endoscopically delivered in the stomachs of 10 H. pylori-positive patients.
Based on a prospective, controlled trial, intragastric violet light phototherapy is safe and feasible and may demonstrate a novel approach to H. pylori eradication, especially in patients who have failed standard antibiotic therapy.
3.4. Vaccine
All H. pylori species in the stomach were positive for urease, which catalyzes urea hydrolysis. UreB is the relatively conserved unit of urease enzyme activity and it is highly antigenic and is important for the survival and survival of bacteria in the acidic conditions of the stomach. UreI, a urea channel protein of H. pylori, is a key factor for bacterial colonization in the acidic mammalian stomach. In one study, a polyclonal vaccine was designed by splicing two antigenic fragments (UreB and UreI) of H. pylori and the cholera toxin B subunit (CTB), resulting in a significant protective effect. reported against H. pylori challenge in BALB/c mice.
Both intramuscular and oral polyepithelial antigens, UreI and UreB, with CTB are immunoprotective against H. pylori challenge, and oral administration has a higher rate of infection protection against H. pylori with H. pylori.
Recently, a reverse vaccination method is used to predict potential vaccine candidates against H. pylori and search for novel antigens using computational or bioinformatics methods. In this study, 5 epithelial antigens including adhesion protein babA, sabA, omp16, iron transport protein (III) dicitrate fecA and toxin acellular vacA were prioritized as potential vaccine candidates. ability to fight H. pylori infection.
The use of antibiotics as first-line therapy may be appropriate if they are selected based on national studies of local and regional patterns of antibiotic resistance. The development of alternative antibiotics to eradicate H. pylori would be invaluable progress, although it would take years before that to evaluate these potentially interesting molecules in humans.
Adjuvant treatment with probiotics is recommended due to immunomodulation, stimulation of mucin production and inhibition of H. pylori colonization and persistence. On the other hand, potential options such as medicinal plants, photodynamic therapy and vaccines are still in the experimental stage.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
1. Lv ZF, Wang FC, Zheng HL, Wang B, Xie Y, Zhou XJ, Lv NH. Meta-analysis: is combination of tetracycline and amoxicillin suitable for Helicobacter pylori infection? World J Gastroenterol . 2015; 21:2522-2533. [PubMed] [DOI]
2. Hajimahmoodi M , Shams-Ardakani M, Saniee P, Siavoshi F, Mehrabani M, Hosseinzadeh H, Foroumadi P, Safavi M, Khanavi M, Akbarzadeh T. In vitro antibacterial activity of some Iranian medicinal plant extracts against Helicobacter pylori. Nat Prod Res . 2011; 25 :1059-1066. [PubMed] [DOI]
3. Buzás GM . Metabolic consequences of Helicobacter pylori infection and eradication. World J Gastroenterol . 2014; 20 :5226-5234. [PubMed] [DOI]
4. Gu H , Li L, Gu M, Zhang G. Association between Helicobacter pylori Infection and Chronic Urticaria: A Meta-Analysis. Gastroenterol Res Pract . 2015; 2015 :486974. [PubMed] [DOI]
5. Ben Chaabane N , Al-Adhba HS. Ciprofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: A randomized trial. Indian J Gastroenterol . 2015; 34 :68-72. [PubMed]
6. Olokoba AB, Obateru OA, Bojuwoye MO. Helicobacter pylori eradication therapy: A review of current trends. Niger Med J . two thousand and thirteen; 54 :1-4. [PubMed] [DOI]
7. Maliheh Safavi, et al., Treatment of Helicobacter pylori infection: Current and future insights. World J Clin Cases. Jan 16, 2016; 4(1): 5-19