This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
The application of artificial intelligence in Barrett's esophagus dysplasia and early esophageal adenocarcinoma has always been evaluated to bring high efficiency in diagnosis. As a result, the treatment becomes more precise and effective.
Abbreviation:
EC: Esophageal cancer
AI: artificial intelligence
Barrett esophagus (BE)
1. Overview of the application of artificial intelligence to gastrointestinal endoscopy
Due to the rapid progression and poor prognosis of esophageal cancer (EC), the early detection and diagnosis of esophageal cancer is of great value in improving the prognosis for patients. However, early endoscopic detection of esophageal cancer, especially Barrett's dysplasia or esophageal squamous dysplasia, is difficult. Therefore, the requirement for a more effective method to detect early esophageal cancer features has led to intensive research in the field of artificial intelligence (AI). Deep learning and memory techniques (DL) have brought breakthroughs in image, video and other aspects of processing, while complex neural networks (CNN) have paved the way for the development of Displays high-resolution endoscopic images and videos. Many studies on complex neural networks in early esophageal cancer endoscopic image analysis show excellent performance including sensitivity, specificity, and gradual progression from in vitro image analysis. for grading to real-time detection of early esophageal tumors in practice.



2. Barrett's dysplasia and early esophageal adenocarcinoma
Artificial intelligence based on white light endoscopy (WLE) and NBI narrowband endoscopy system, there are some limitations to recognize early cancerous lesions associated with Barrett's esophagus by WLE, a common technology. High-definition WLE (HD-WLE) and the NBI endoscopy system were once considered to improve the accuracy of diagnosing early cancerous lesions associated with Barrett's esophagus. But the improvement has yet to satisfy endoscopists. This situation stimulated the development of a CAD system for early cancerous lesions in Barrett's esophagus based on a supervised ML blood learning algorithm. However, this system still has difficulty in identifying early cancerous lesions associated with Barrett's esophagus and selecting biopsy sites.
To solve those problems, Ebigbo et al established a CAD system based on deep learning algorithms. The accuracy of the system using HD-WLE is better than that of the general endoscope system. Furthermore, the system shows the ability to locate lesions and the regional matching rate between lesions by the system and local experts up to 72%. In general, the specificity of NBI is higher than that of conventional WLE.
Compared with HD-WLE, the system has no obvious advantage when using NBI system. However, there was a common problem in the above studies i.e., the same image dataset was used in both training and validation phases. This obviously cannot reflect clinical practice, so it is very important to use different imaging datasets for training and validation.
De Groof et al used different HD-WLE images for training and testing, the results showed that the sensitivity and specificity of the system was significantly higher than that of general endoscopists . The combination of AI and HD-WLE/NBI, widely used in the clinic, performs well in the diagnosis of early tumor lesions associated with BE and outperforms the general endoscopes . However, in different studies, the accuracy of the CAD system in lesion delineation and the criteria for assessing the ability to locate the lesion are quite conflicting. More high-quality studies are needed in the future.
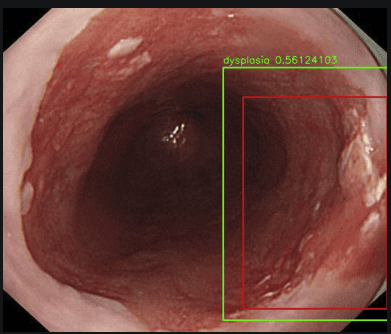
3. AI real-time diagnosis
CAD system optimization based on previous research and applied to clinical real-time detection for the first time. While 14 Barrett's cancer patients underwent endoscopic examination, 62 endoscopic images (36 early esophageal carcinoma and 26 non-dysplastic Barrett's esophagus) were taken with the CAD system for real-time classification. , the results showed sensitivity and specificity of 83.7% and 100%, respectively. There were no significant differences between the system and the experienced endoscopists. However, there are still some shortcomings in this study. First, the number of patients and images is low. Second, the system still uses images for diagnosis, not video for real-time detection. Finally, AI's ability to aid in lesion delineation and biopsy guidance remains unproven.
In addition, the CAD system built by Hashimoto et al., can meet clinical real-time detection needs; Unfortunately, the researchers did not verify the system's performance in real-time diagnostics.

4. Esophageal squamous dysplasia and early esophageal squamous cell cancer
AI-based AI based on WLE and NBI: Lugol's pigment endoscopy is the standard screening method for esophageal squamous cell carcinoma, however, due to its low specificity and long duration of consumption. Therefore, new endoscopic techniques need to be applied. Although WLE has been shown to be unsuitable for early esophageal squamous cell carcinoma screening alone, in terms of clinical prevalence some researchers still hope to introduce AI to improve accuracy. WLE accuracy.
Cai et al built a DL-based CAD system and experimented with WLE images. The results show that the accuracy of the system in diagnosing early esophageal cancer is significantly higher than that of the primary and intermediate endoscopists, and there is no significant difference between the system and the physicians. high end endoscopy. The results of Ohmori et al showed that the sensitivity of NBI was higher than that of WLE, but the specificity was lower, and there was no significant difference between the overall performance of the system and the endoscopists. The results of Horie et al. are similar to those of Ohmori.
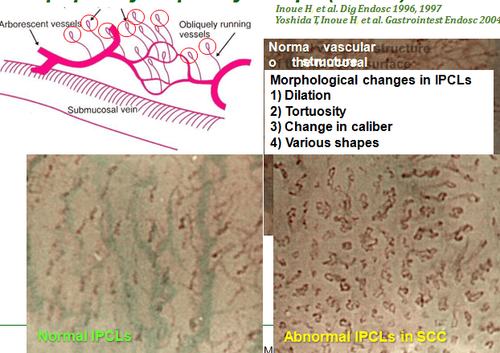
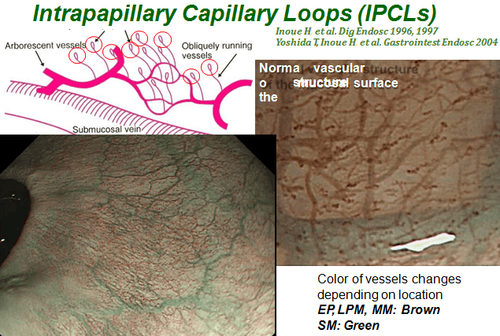
In recent years, it has been recognized that the capillary loop structure observed on esophageal endoscopy (IPCL) represents an endoscopically visible feature of esophageal squamous cell neoplasms. and morphological changes are closely related to the depth of invasion of melanoma. The NBI-based IPCL classification proposed by the Japanese Society of Endoscopy has been widely used in clinical practice because of their ease of understanding. However, IPCL classification still requires sufficient experience and interpretation is still subjective. Therefore, to classify IPCL more objectively and help less experienced endoscopists make full use of NBI, combining NBI with AI will be the best solution.
Zhao et al analyzed magnified NBI images and showed that the diagnostic accuracy of the CAD system was better than that of the junior and intermediate endoscopists and there was no significant difference between the this system with senior endoscopists. However, this study only focused on IPCL classification and did not further verify the accuracy of the tumor depth-invasion system. For early ESCC, accurate determination of tumor invasive depth is a prerequisite for selecting appropriate treatment. Nakagawa et al used unmagnified endoscopic imaging to examine the CAD system and found that the sensitivity of this system for the diagnosis of invasive submucosal, carcinoma was up to 200 μm (EP- SM1) was higher than that of the endoscopist, but the specificity was lower. There were no significant differences between the system and the endoscopists based on magnified endoscopic images.
Further analysis showed that the system performed well in the diagnosis of cancer localized in the EP/lumbar layer (LPM) and there was no significant difference compared with the expert endoscopists. However, the sensitivity of the SM1/myomuscular (MM)/submucosal tumor diagnosis system is poor, as is the performance of the endoscopists. In the diagnosis of tumors invading the SM2/3 submucosa, the sensitivity of this system is slightly higher than that of expert endoscopists.
The benefits of artificial intelligence in Barrett's esophagus and early-stage esophageal adenocarcinoma play a very important role in helping to provide an accurate diagnosis so that appropriate treatment can be given. with each medical condition.
Department of Gastroenterology - Vinmec International General Hospital is developing services for screening and early detection of gastrointestinal cancer combined with clinical and paraclinical examination to bring the most accurate results to patients. thereby giving positive treatment direction to help patients control their health condition early.
The hospital visit not only brings accurate diagnosis and treatment results thanks to a team of doctors with many years of experience, combined with a system of modern equipment with NBI endoscopes with anesthesia. . Peripheral blood count (laser counter). Automated prothrombin time test. Activated Partial Thromboplastin Time (APTT) test using an automated machine. General abdominal ultrasound ... but the hospital also has an extremely civilized and polite examination space to bring comfort to the patient.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [PubMed] [DOI] Hur C, Miller M, Kong CY, Dowling EC, Nattinger KJ, Dunn M, Feuer EJ. Trends in esophageal adenocarcinoma incidence and mortality. Cancer. 2013;119:1149-1158. [PubMed] [DOI] Thrift AP. The epidemic of oesophageal carcinoma: Where are we now? Cancer Epidemiol. 2016;41:88-95. [PubMed] [DOI] Lu-Ming Huang, Wen-Juan Yang, Zhi-Yin Huang, Cheng-Wei Tang, Jing Li, Artificial intelligence technique in detection of early esophageal cancer, World J Gastroenterol. Oct 21, 2020; 26(39): 5959-5969