This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalRecent advances in artificial intelligence (AI) can help gastroenterologists identify potentially dysplastic areas in Barrett's esophagus and perform targeted biopsies , thereby reducing procedure time, sedation time, and patient risk along with maximizing potential biopsy output.
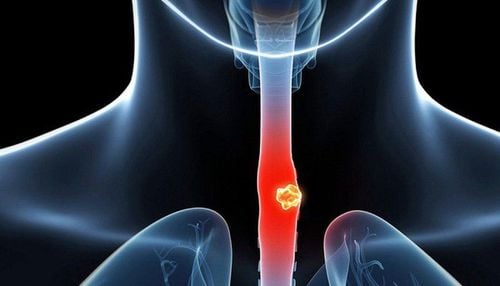
1.Esophageal cancer overview
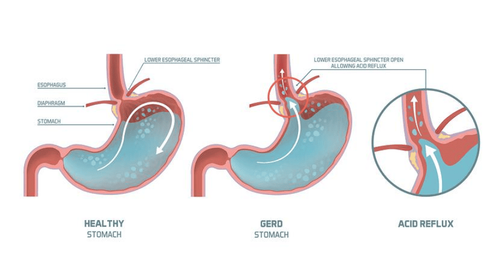
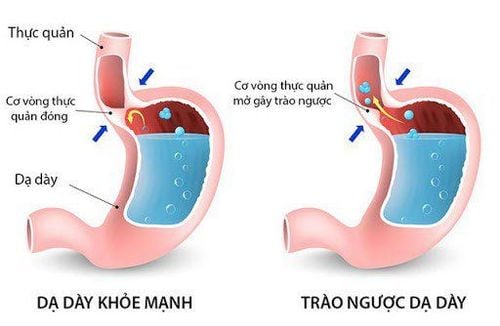
Esophageal cancer remains one of the top ten causes of cancer-related death in the United States. The main risk factor for esophageal adenocarcinoma is the presence of Barrett's esophagus (BE).
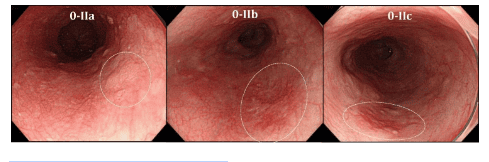
Currently, the identification of early dysplasia in patients with Barrett's esophagus requires an experienced endoscopist to perform diagnostic endoscopy with random 4-quadrant biopsies taken every 1-2 cm of use appropriate follow-up intervals. Endoscopists have considerable difficulty distinguishing between the different forms of Barrett's esophagus as well as early adenocarcinoma due to subtleties in the texture and color of the mucosa. This obstacle makes multiple random biopsies necessary for appropriate follow-up and diagnosis.
2.Recent Advances in Diagnostic Endoscopy
Recent advances in artificial intelligence (AI) can help gastroenterologists identify potentially dysplastic areas in Barrett's esophagus and perform targeted biopsies , thereby reducing procedure time, sedation time, and patient risk along with maximizing potential biopsy output.
Although the use of AI represents an exciting frontier in endoscopic medicine, recent studies are limited by selection bias, generalization, and lack of robustness for universal use. Before AI can be reliably used for Barrett's esophagus in the future, these issues need to be fully addressed and tested in prospective, randomized trials. Only after that is achieved will the benefits of AI in people with Barrett's esophagus be fully realized. Only after that is achieved will the benefits of AI in people with Barrett's esophagus be fully realized.
Screening and surveillance in patients with Barrett's esophagus remains a matter of accuracy and compliance. This occurs despite the advice and advances in endoscopic imaging. Artificial intelligence (AI) algorithms aid endoscopic assessment of Barrett's esophagus by identifying potential targets for biopsy. This can be achieved by increasing endoscopic efficiency and diagnostic accuracy by reducing procedure time. AI in Barrett's esophagus has been developed by expert endoscopists and appears to work similarly among them. At this point, the benefits of AI in Barrett's esophagus can be used by endoscopists and non-expert trainees to maximize endoscopic evaluation of Barrett's esophagus.
3.Risk factors for esophageal cancer
In 2020, the United States is estimated to record more than 18,000 new cases of esophageal cancer and more than 16,000 deaths. Furthermore, esophageal cancer remains in the top 10 cancers diagnosed and causes cancer deaths nationally. A common risk factor for esophageal adenocarcinoma (EAC) is the presence of Barrett's esophagus. Currently, early identification of dysplasia requires an experienced endoscopist to perform diagnostic laparoscopy consisting of random 4-quadrant biopsies taken every 1-2 cm during appropriate follow-up intervals. based on the absence or presence of dysplasia seen in random biopsies.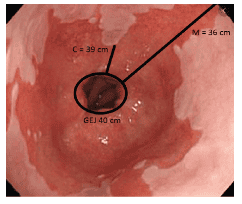
4.Difficulty in diagnosing early stage esophageal cancer
Unfortunately, adherence to this recommendation remains inconsistent, especially with low-grade dysplasia. The subtle appearance is difficult to discern by conventional endoscopy and its discontinuous nature can make it difficult to accurately biopsies areas of tissue pathology to confirm or rule out the diagnosis.
In addition, there is considerable difficulty for endoscopists in distinguishing Barrett's esophagus with low-grade dysplasia from high-grade dysplasia (HGD) or early adenocarcinoma. To combat this, high-definition white light, narrow band imaging (NBI), probe-based confocal endoscopy (pCLE), volumetric laser endoscopy (VLE), and optical computed tomography among others have all been tested and used to increase biopsies yielding accurate diagnostic results.
However, early-stage esophageal cancer is often flat and difficult to distinguish from surrounding non-dysplastic Barrett's mucosa, even with these endoscopic advances. The rate-limiting step between these technologies is that they are operator dependent, requiring hand-eye coordination to distinguish and biopsies suspect areas, often taking years to acquire skill sets. necessary. Theoretically, artificial intelligence (AI) could help with this by using deep learning methods to identify and process - in real time - endoscopic data that might not be human. Conscious assessment such as subtle changes in color and texture to aid in targeted biopsies rather than random biopsies.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Please continue reading: The role of artificial intelligence in Barrett's esophagus (Part 2)