This is an automatically translated article.
Article written by MSc Nguyen Ngoc Khanh - Head of Department of Gastroenterology - Urology - Robotic Surgery & Pediatric Surgery, Vinmec Times City International General Hospital.
The article aims to provide basic information to customers about the concept of gastroesophageal reflux disease, disease manifestations, risks brought by the disease, prevention and treatment.
1. General concepts
Gastroesophageal reflux is a normal physiological phenomenon experienced by most people, especially after meals. Gastroesophageal reflux disease (GERD) occurs when the amount of gastric juice that backs up into the esophagus exceeds normal limits, causing symptoms with or without damage to the lining of the esophagus.
Patients with GERD may present with typical and atypical symptoms. Typical symptoms include: heartburn, reflux, and difficulty swallowing. Atypical symptoms include: noncardiac chest pain, asthma, pneumonia, hoarseness and aspiration cough.
25-40% of healthy American adults have symptoms of GERD, the most common clinical manifestation of which is heartburn (pyrosis) at least once a month. 7-10% of adults experience these symptoms on a daily basis.
GERD is a common disease with a high prevalence. Statistically the prevalence of GERD ranges from 18.1% to 27.8% in North America, 8.8% to 25.9% in Europe, 2.5% to 7.8% in East Asia, 8, 7% to 33.1% in the Middle East, 11.6% in the Middle East in Australia and 23.0% in South America.
In most people, intrinsic defense mechanisms either limit the amount of harmful substances entering the esophagus or rapidly clear it from the esophagus so symptoms and irritation of the lining of the esophagus are minimized (eg. Examples of this mechanism are the lower sphincter and peristaltic activity of the esophagus). When these protective mechanisms fail or become overloaded, the esophagus becomes flooded with acid or bile for long periods of time, then gastroesophageal reflux disease (GERD).
2. How does gastroesophageal reflux disease manifest?
Patients with GERD present different symptoms, typical and atypical.
Typical (esophageal) symptoms include: Heartburn Reflux Difficulty swallowing Atypical (extraesophageal) symptoms include: Chest pain (not due to cardiovascular disease) Asthma Pneumonia Hoarseness Cough, Choking Patients often have multiple episodes of reflux daily manifesting in the form of heat behind the sternum, heartburn, coughing at night, pneumonia, bronchospasm, laryngitis, voice changes. In addition, objective evidence of esophageal injury can be seen on esophagoscopy as indicated by degrees of esophagitis.
Tests are of little help in diagnosing GERD. Esophageal activity measurement and pH monitoring are considered essential before performing anti-reflux surgery. Endoscopy revealed that 50% of patients did not have esophagitis. The only way to determine if there is abnormal reflux and if the symptoms are actually caused by GERD is through pH monitoring.
Achalasia may present with heartburn. Only esophageal activity measurement and pH monitoring can be used to distinguish achalasia from GERD. Treatment is completely different with these 2 diseases.
GERD is treated step by step based on lifestyle modification, gastric secretion control with medical treatment or surgery.
3. Anatomy of the esophagus, stomach
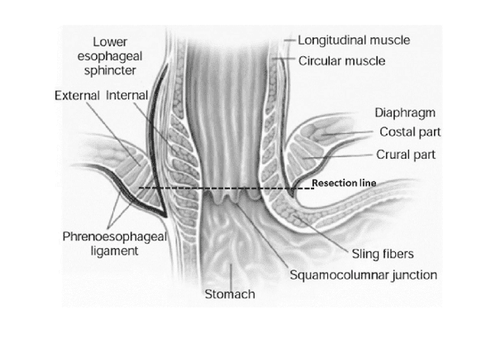
The anatomy of the esophagus, stomach, and esophagogastric junction is important in understanding the pathogenesis of reflux.
The esophagus is divided into 3 parts: neck, thorax, and abdomen. The wall of the esophagus is made up of layers of longitudinal muscles and an inner ring. The proximal third of the esophagus is striated muscle, which converts to smooth muscle in the distal two parts. The proximal esophagus contains the upper esophageal sphincter (UES).
When the thoracic esophagus enters the abdominal cavity through the diaphragmatic foramen, it becomes the abdominal esophagus.
The transition is located in the abdomen with the gastric bulge forming the angle of His. The angle of His and the length of the abdominal esophagus both contribute to normal esophageal closure when intra-abdominal and intra-abdominal pressures are high.
The lower esophageal sphincter, or more precisely the high-pressure zone, is the distal part of the esophagus (3-5 cm in adults). Maintaining an adequate intra-abdominal high pressure zone is important in preventing GERD.
GERD due to the absence of one or more of these anatomical features. Correct surgical treatment requires a complete pre- and intraoperative evaluation and correction of all such defects.
4. Pathophysiology
Diagrammatically, the esophagus, lower esophageal sphincter (LES), and stomach can be visualized as a simple water tube. The esophagus functions as a pump, the LES as a valve and the stomach as a reservoir. GERD can be from any component of the system. Poor esophageal motility reduces acid clearance. The dysfunctional LES allows the reflux of large amounts of gastric juice. Gastric retention both leads to GERD. Determine which of these components is defective in order to apply effective therapy.
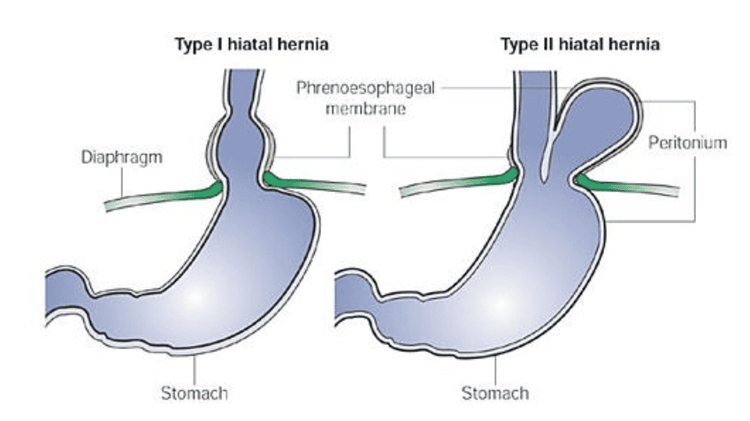
4.1 Diaphragmatic Hernia When discussing the mechanisms for GERD, the issue of diaphragmatic hernia must be mentioned. A hiatal hernia can be seen frequently in patients with reflux disease; however, it has been shown that not all patients with hiatal hernia have symptomatic reflux.
4.2 Obesity is a contributing factor Several studies have shown that GERD is very common in patients with obesity and a high body mass index (BMI)
5. What are the consequences of gastroesophageal reflux disease?
If left unchecked, gastroesophageal reflux disease, which can lead to serious problems including esophagitis, Barrett's esophagus, esophageal stricture and esophageal cancer.
5.1 Esophagitis
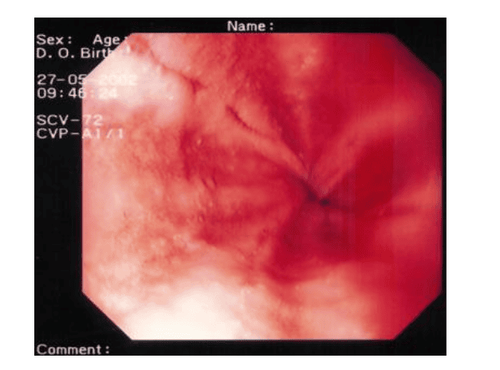
When stomach acid repeatedly comes into contact with the lining of the esophagus, it causes inflammation, which can include erosion or ulcers. Esophagitis can cause symptoms such as heartburn, chest pain, difficulty swallowing, or bleeding.
5.2 Barrett's esophagus
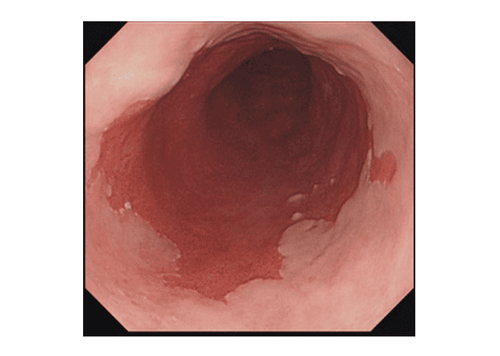
Barrett's esophagus accounts for about 10% of people with persistent GERD. It is a risk factor for esophageal cancer. Damage from acid reflux can cause abnormal changes in the lining of the esophagus. The normal squamous cells of the esophagus are replaced by another type of abnormal cell. These abnormal cells are similar to those normally found in the lining of the small intestine.
People who have had heartburn for many years may be at risk for Barrett's esophagus. Barrett's esophagus is common in middle-aged and older people. Men more than women.
Barrett's esophagus was diagnosed by endoscopy to evaluate the lining of the esophagus and take a biopsy for examination. Experts recommend endoscopy to examine Barrett's esophagus in people with risk factors, such as persistent heartburn (more than 10 years), Caucasian race, male gender, and being overweight. Barrett screening, not recommended for the general population.
Although uncommon, Barrett's esophagus can lead to esophageal cancer. Because of the risk of cancer, people with Barrett's esophagus are often examined regularly with endoscopy.
The goal of treatment for Barrett's esophagus is to prevent further damage by stopping acid reflux from the stomach. Proton pump inhibitors such as Omeprazole®, Nexium®, Protonix®, Prevacid®, Prilosec®, and Aciphex® and others are the mainstay of treatment. These drugs reduce the amount of acid produced by the stomach. In some patients, surgery to strengthen the sphincter, or "valve" between the esophagus and stomach, is an option to prevent reflux.
5.3 Esophageal stricture
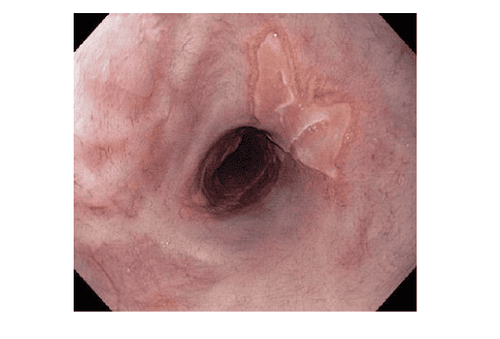
The damaged lining of the esophagus becomes scarred, causing narrowing of the esophagus. These lesions prevent food and liquid from reaching the stomach.
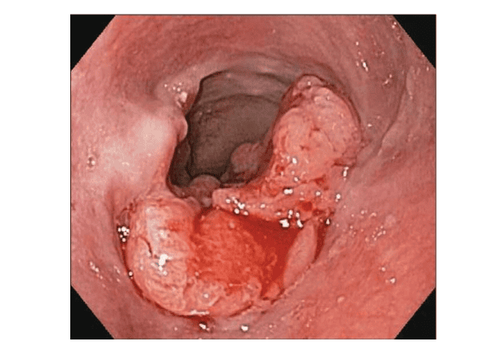
5.4 Esophageal cancer Cancer that begins in the esophagus is divided into two main types:
Squamous cell carcinoma : This cancer is usually in the upper and middle parts of the esophagus. The risk factors are smoking and strong alcohol. Adenocarcinoma: This type of cancer is usually in the lower part of the esophagus. It may arise from Barrett's esophagus. Esophageal cancer, in its early stages, often has no symptoms. Difficulty swallowing is the most common symptom of esophageal cancer. As the cancer grows, it narrows the opening of the esophagus, making swallowing difficult and/or painful.
6. Treatment of GERD
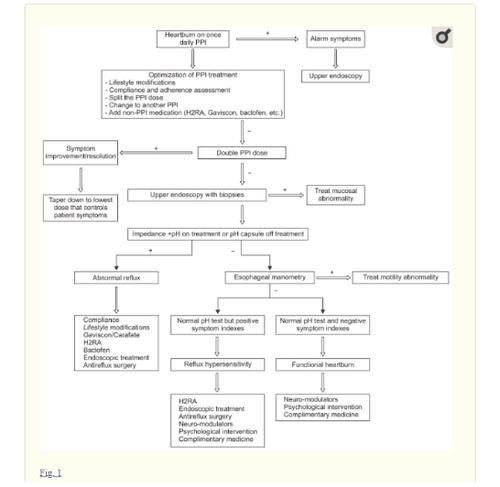
Most patients with typical GERD symptoms are treated empirically with proton pump inhibitors (PPIs) and do not undergo diagnostic testing. However, in patients with alarming symptoms such as dysphagia, dysphagia, dysphagia (odynophagia), anorexia, weight loss, and upper gastrointestinal bleeding, examination with upper gastrointestinal endoscopy is warranted.
6.1 Available treatment modalities for gastroesophageal reflux disease Lifestyle changes:
Medications:
Surgery:
Interventional endoscopy:
6.2 Treatment for nocturnal gastroesophageal reflux disease Avoid eating near bedtime (3h) Elevate the head of the bed Avoid lying on the right side Turn off the lights at bedtime, avoid sleep disturbance Treat with a proton pump inhibitor (PPI) before dinner if symptoms are mainly at night Divide PPI dose into morning and evening before meals. Add: H2-antagonist, Carafate; Gaviscon...before bed consider non-medical therapy 6.3 Available PPIs Omeprazole Esomeprazole Lansoprazole Rebaprazole Dexlanprazole Omeprazole with Sodium bicarbonate 6.4 Steps to optimize PPI drug therapy Lifestyle changes Compliance Dose and duration Split PPI Dose Switching PPIs Persistent heartburn is defined as GERD unresponsive to a double dose of PPI for at least 8 weeks. Successful treatment of persistent heartburn depends on the underlying mechanism.
7. Surgical treatment
Usually reserved for patients with reflux complications such as recurrent or refractory esophagitis, strictures, Barrett's esophagus, persistent "reflux symptoms" despite acid suppression or asthma. The patient cannot tolerate medication, is not compliant with medication, or is dependent on it and does not want to take it for the rest of his life.
Nissen fundoplication Surgery Can be performed with laparoscopic or robotic surgery. Real surgery uses a large gastric aneurysm to create an anti-reflux valve.
Linx Magnetic Ring Surgery Can be performed with laparoscopic or robotic surgery. Surgery uses a magnet ring, placed around the lower esophagus to strengthen the esophageal sphincter.
In case reflux disease makes you uncomfortable, does not go away for a long time or shows signs such as difficulty swallowing, choking, dull pain, you need to go to a gastroenterologist immediately for treatment intervention. timely.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.