This is an automatically translated article.
Hepatic veno-occlusive disease is caused by endothelial damage, resulting in non-thrombotic obstruction of the hepatic venules and hepatic sinuses rather than the hepatic vein or inferior vena cava (eg. as in Budd-Chiari syndrome). The following article will clarify more about the dangers of hepatic vein occlusion or hepatic portal vein occlusion if it is not diagnosed and detected early.
1. What is Hepatic Venous Obstruction and Budd Chiari Syndrome?
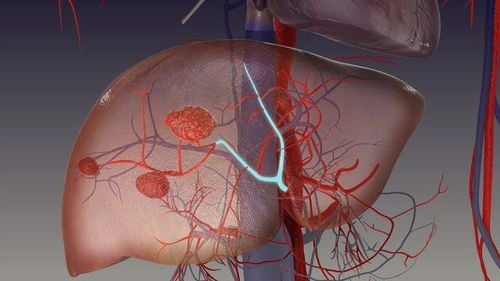
Budd Chiari syndrome – one of the most common syndromes of hepatic venous occlusion (or hepatic portal vein occlusion) is a condition in which the hepatic veins (veins that drain the liver) are blocked or narrowed by a clot. blood clots (mass of blood cells). This blockage causes blood to back up into the liver, and as a result the liver grows larger than normal. The spleen (an organ located in the upper left side of the abdomen that helps fight infections by filtering the blood) may also grow larger. Budd-Chiari syndrome can also cause other health problems such as:
Portal hypertension (increased pressure in the portal vein, which carries blood from the intestines to the liver). Esophageal varices (twisted veins in the esophagus, also known as the "food pipe"). Ascites (accumulation of fluid in the abdomen). Cirrhosis (Scarring of liver cells). Varicose veins (abnormal and swollen blood vessels) in the abdomen and/or rectum.
2. Causes and symptoms of Budd Chiari . syndrome
2.1. Causes Budd Chiari syndrome in particular or hepatic vein occlusion in general can be caused by conditions and situations that cause a normal person's blood to clot (form blockages) with other causes: mainly:
myeloproliferative diseases (diseases that affect the blood and bone marrow), including polycythemia vera (the body makes too many red blood cells) and thrombocytopenia ( the body produces too many platelets). Sickle cell disease (a blood disease in which red blood cells change shape from round to sickle). Inflammatory bowel disease (a group of disorders that cause irritation and swelling of the digestive tract). Mothers in pregnancy 2.2. Symptoms Symptoms of Budd Chiari syndrome include:
Upper abdominal pain. Ascites (painful swelling in the abdomen caused by excess fluid). Jaundice (skin, whites of eyes, and mucous membranes turn yellow). The liver is large and tender. Bleeding in the esophagus. Edema (swelling) in the legs. Liver failure. Hepatic encephalopathy (decreased brain function due to liver disease). Vomiting. Large spleen. Fatigue (even the sick person may feel extremely tired). Among the symptoms of hepatic venous occlusion, ascites and hemodynamic changes of the portal venous system are the most dangerous.
Ascites : Ascites is the result of a combination of disorders. The causes of ascites are portal hypertension, increased vascular permeability, decreased intravascular oncotic pressure, and impaired water metabolism due to hormonal disturbances, such as aldosterone, ADH, and sex hormones. Recently, it has been suggested that ascites has the involvement of lymphatic circulation disorders. Ascites accounts for 30-50% in Budd Chiari syndrome, when ascites is large, it will compress the abdominal organs, restrict movement of the diaphragm, causing difficulty breathing, compressing the veins, making blood difficult. circulate. Therefore, in many cases, surgical intervention is required.

Hình ảnh người bệnh mắc hội chứng Budd Chiari
Changes in hemodynamics of the portal system: The portal vein and the superior hepatic vein join together in the hepatic sinus. The same blood flow to the hepatic sinuses with the portal vein has the hepatic artery. Thus, the pressure in the hepatic sinuses will be governed by two components: portal pressure and hepatic artery pressure. The normal pressures in the portal vein and the pressure in the hepatic sinuses are between 7 and 10 mmHg. The venous pressure on the liver is 5-8 mmHg. Depending on the location of the occlusion, the pressure measured at the above positions will be different. If the obstruction is in front of the sinus, the pressure measured in the spleen will be very high, while the pressure in the sinus is normal, there is a large difference in pressure measured in the axilla and in the sinus. Common causes of portal vein occlusion outside the liver (such as congenital portal vein occlusion, disseminated portal vein thrombosis and splenic vein occlusion...), intrahepatic portal vein occlusion (cirrhosis caused by cirrhosis) parasites and portal hypertension not due to cirrhosis, etc.).
When the sinus is blocked, the pressure measured in the axilla is very high and the pressure in the sinus is also high, approximately without a significant pressure difference between the pressure in the axilla and the sinus. Common types of obstruction in the liver (alcoholic cirrhosis, cirrhosis after necrotizing hepatitis, cirrhosis due to malnutrition, cholestatic cirrhosis, cirrhosis in cancer ...) and obstruction in the liver or later liver (suppressive hepatic venous occlusion: Budd Chiari, inferior vena cava and portal hypertension secondary to cardiac diseases...). Based on the pressure change, one can accurately diagnose the location of the intrahepatic or extrahepatic obstruction, on that basis, an appropriate surgical treatment method is selected.
3. Diagnosis and treatment of hepatic vein occlusion
3.1. Diagnosis Clinical diagnosis:
Portal hypertension represents a pathological state of multiple symptoms
and clinical signs of a severe stagnation of the portal system.
Splenomegaly: A common phenomenon, accounting for 66-80% of patients. The spleen can be very enlarged, up to grade 4 -5. The collateral circulation: Glossy blue veins emerge under the skin from around the navel to the chest wall and down to the groin, more visible when the patient is sitting. Hemorrhoids: This is a manifestation of the stretching of the annulus around the rectum. However, hemorrhoids are not typical symptoms of portal hypertension and are not frequent signs Ascites: Common in the period of severe circulatory stasis, accounting for 20-45%. The ascites is lemon yellow, greenish, and the Rivalta reaction is negative. Gastrointestinal bleeding: Due to rupture of varicose veins at the portal-aortic annulus. The most common is the lower third of the esophagus and stomach. accounted for 40-50%. The patient has a marked hemorrhagic syndrome. May be repeated many times. Subclinical diagnosis
Contrast Esophageal X-ray: Wolf in 1928 and Schatzki in 1931 gave patients a baryte sulfate contrast agent mixed with an adhesive. Place patient in standing and lying position for X-ray, take 6-10 seconds after patient takes a sip of baryte. Should be taken in between episodes of vomiting blood. On radiographs, ridges are seen along the esophagus: These are distended esophageal veins exposed into the lumen of the esophagus. Spleen-portal : Contrast X-ray of the portal vein system (Bulven and Sheval) by inserting a needle into the spleen injecting contrast agent (visotract, cardiotrast, etc.), through which to image the splenic-portal venous system. The results of this method give us the image and degree of dilatation of the portal vein and the poor, fibrous image of the portal vein branches that drain into the liver (helping us to indirectly evaluate the cirrhosis). Distal liver: Take X-ray from a distance to evaluate the size of the liver. When endoscopically, it can be seen that in the wall of the esophagus, especially in the posterior wall of the lower third of the esophagus, there are prominent venous tufts, pale green, distended, sometimes clearly curved. In some cases, esophageal veins can be seen ruptured, blood oozing out, or mucosal abrasions can be seen in the esophageal wall. Measurement of portal venous pressure: Usually measured by the following methods: Indirect measurement through splenic puncture (because portal vein and splenic vein do not have valves, so splenic pressure and portal venous pressure are always equal, rarely there is a small insignificant difference); Measure directly during surgery by inserting a needle straight into the portal vein; Esophageal venous pressure measurement through esophageal endoscope; Measure free hepatobiliary pressure and hepatobiliary pressure by right cardiac catheterization (Friedman and Weiner 1961). Laparoscopy and liver biopsy: To accurately assess the type and extent of cirrhosis. Quantification of total protein ratio (albumin and globulin): A decrease in the amount of albumin in the blood below 3% is a sign of impaired liver function. Blood tests: Blood tests often give low results, sometimes far from normal because the patient has severe anemia, for example, red blood cells may be below 1,000,000/mm3, white blood cell count less than 2000/mm. mm3, platelets 40,000-50,000/mm3, hematocrit 10-15%.

Tắc nghẽn dòng chảy tĩnh mạch trong gan trong hội chứng Budd-Chiari
3.2. Budd-Chiari syndrome treatment Budd-Chiari syndrome treatment is designed to dissolve blood clots and help you improve blood flow in your liver. Treatments will usually include medication, non-surgical procedures, and surgery: Drug therapy: Your doctor will prescribe medication to dissolve the blood clot. In addition, the blood thinner warfarin (Coumadin) is often prescribed to prevent future blood clots from reappearing. Procedures: There are two non-surgical procedures used to treat Budd Chiari syndrome: Intravenous streptococcal catheterization and percutaneous angioplasty: Transarticular intrahepatic portal system (TIPS) shunt is an X-ray procedure in which a stent (a tubular device) is placed in the center of the liver to position the liver. re-route the blood stream. During surgery, the radiologist creates a tunnel through the liver with a needle, connecting the portal vein (the vein that carries blood from the digestive organs to the liver) with one of the hepatic veins (three veins leading to the liver). blood from the liver.). A metal stent (a small, hollow tube) is placed in the tunnel to keep the tunnel open. The TIPS procedure reroutes blood flow in the liver and relieves pressure in all abnormal veins, including the intestines and liver.
In percutaneous coronary angioplasty, your doctor will thread a catheter (a thin, hollow tube with a balloon at the end) through your skin and into a blood vessel. The catheter is guided to the area where the clot is located. When the catheter touches the clot, the balloon is inflated to widen the vein. A stent is placed in place to keep the vein open.
Surgery: If the patient has liver failure (the liver is no longer fully functional), a liver transplant is the commonly used treatment. Hepatic venous occlusion (or hepatic portal vein occlusion) is a serious medical condition. and is the major cause of Budd Chiari syndrome. Without prompt treatment, people with complete hepatic vein occlusion can die of liver failure within 3 or 5 years. The survival rate in this case will be increased with a liver transplant. People with partial vein occlusion may live longer, but life expectancy is different for each person in this case.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.