This is an automatically translated article.
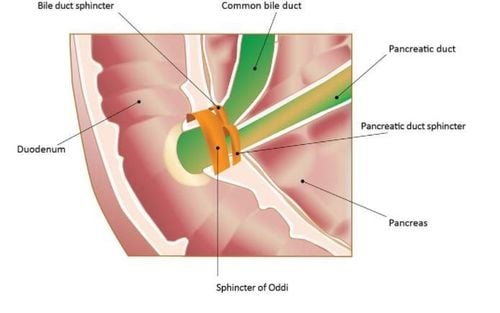
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Sphincter of Oddi dysfunction is a term used to describe a heterogeneous group of pain syndromes caused by abnormalities in the sphincter's ability to contract. Disorders of the biliary and pancreatic sphincter of Oddi are classified into categories I, II, or III, according to the Milwaukee classification.
1. Pain patterns in sphincter of Oddi
Because of the anatomical location of the sphincter of Oddi, patients with sphincter of Oddi disorder often present with recurrent biliary or pancreatic pain. The Rome II diagnostic criteria for biliarygia are severe and stable pain in the right epigastrium and lower abdomen, associated with all of the following:
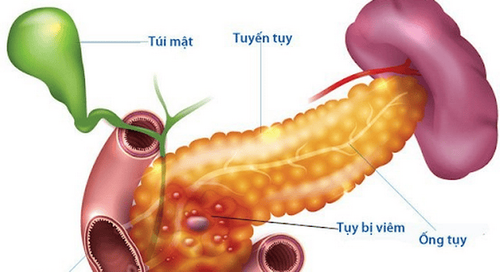
Symptomatic episodes lasting at least 30 minutes with painless episodes in between; Have at least one pain in the past 12 months; Pain that is constant and disrupts daily activities or requires consultation with a doctor; There was no evidence of structural abnormalities to explain the symptoms. Pancreatic pain is described as intermittent, persistent, postprandial pain in the upper abdomen and/or back. It is often assumed in the setting of recurrent acute pancreatitis in the absence of biliary tract disease or anatomical abnormalities. The true incidence of sphincter of Oddi disorders is not known, but intermittent biliary pain occurs in 10%-20% of patients who have had a cholecystectomy. Sphincterotomy, often with endoscopic sphincterotomy, is at the forefront of the management of sphincter of Oddi disorder, and one of the challenges of this condition is determining which patients would benefit from it.
2. Milwaukee classification of pain patterns in sphincter of Oddi Pains due to biliary tract:
Typical biliary tract pain: Liver enzymes (AST, ALT or ALP) > 2 times the normal limit of normal received on at least 2 occasions during episodes of pain. Diluted common bile duct >12 mm in diameter. Prolonged bile drainage time (> 45 min). Class II: Biliary tract pain and one or two of the above criteria. Class III: Only biliary tract pain. Pancreatic sphincter of Oddi disorder:
Type I: Pain-type pancreatitis. Amylase and/or lipase >2 times upper limit of normal on at least 2 occasions during multiple episodes. The pancreatic duct is dilated (pancreatic head > 6 mm, body > 5 mm). Prolonged pancreatic drainage time (> 9 min). Type II: Type of pancreatic pain and one or two of the above criteria. Type III: Pancreatic pain only.
However, in a cohort of 59 patients, Majeed et al found no difference between the diameters of the common bile duct before and after cholecystectomy. Since the upper normal limit of the common bile duct diameter is 7 mm, resection of 12 mm has the potential to lead to a large number of patients being misdiagnosed. In addition, differences in basal pressure and sphincter response between the biliary and pancreatic parts of the sphincter of Oddi have led to requests to remove this dual classification system in favor of a single holistic system. best.
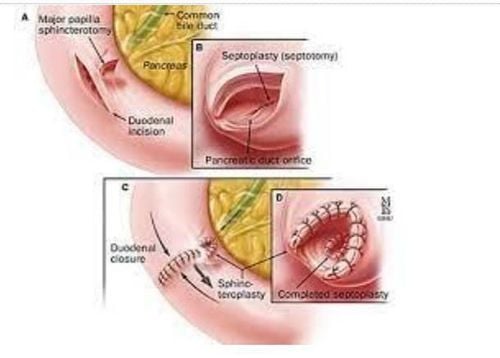
4. Different and common management for each disorder of the sphincter of Oddi 4.1. Various management Some researchers have found that manometry and resection of both biliary and pancreatic sphincters are required to adequately assess and treat sphincter of Oddi disorders. In pancreatic sphincter of Oddi disorders up to 88% of patients would benefit from sphincterotomy. As a result, there have been calls from several regions for the removal of the current classification system in favor of a holistic system that includes biliary and pancreatic types. Future work should aim to understand the underlying mechanisms of the relationship between sphincter of Oddi disorder and pancreatitis as well as to identify patient factors that will help predict benefit from endoscopic therapy. For patients with types II and III, the benefit of endoscopic sphincterotomy is lower. These patients should be evaluated more thoroughly before performing laparoscopic sphincterotomy. Some researchers have found that manometry and resection of both biliary and pancreatic sphincters are required to adequately assess and treat sphincter of Oddi disorder.
4.2. Common Management Various mechanisms have been recognized, but the exact role of the sphincter of Oddi dysfunction in the pathophysiology of acute pancreatitis remains unknown. There is also an association between sphincter of Oddi disorder and chronic pancreatitis but it is not clear whether this is a cause-and-effect relationship. Management of the sphincter of Oddi disorder is aimed at resection of the sphincter, usually endoscopic sphincterotomy (ES). Patients with type I sphincter of Oddi disorder will benefit from endoscopic sphincterotomy in 55% to 95% of cases. Sphincter of Oddi manometry is not necessary before endoscopic sphincterotomy in type I sphincter of Oddi disorders. For type II and III patients, the benefit of endoscopic sphincterotomy is lower. These patients should be evaluated more thoroughly before performing laparoscopic sphincterotomy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
1. Toouli J, Roberts-Thomson IC, Dent J, Lee J. Sphincter of Oddi motility disorders in patients with idiopathic recurrent pancreatitis. Br J Surg. 1985; 72 :859–863. [PubMed] [Google Scholar]
2. Varadarajulu S, Hawes R. Key issues in sphincter of Oddi dysfunction. Gastrointest Endosc Clin N Am. 2003; 13:671–694. [PubMed] [Google Scholar]
3. Petersen BT. An evidence-based review of sphincter of Oddi dysfunction: part I, presentations with "objective" biliary findings (types I and II) Gastrointest Endosc. 2004; 59 :525–534. [PubMed] [Google Scholar]