This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
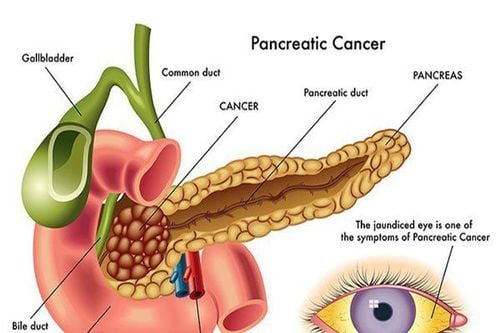
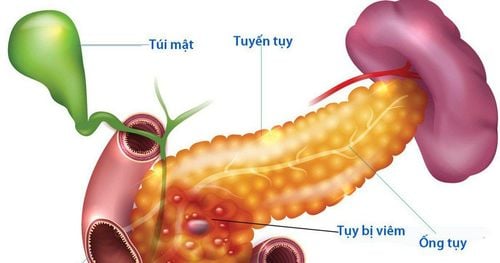
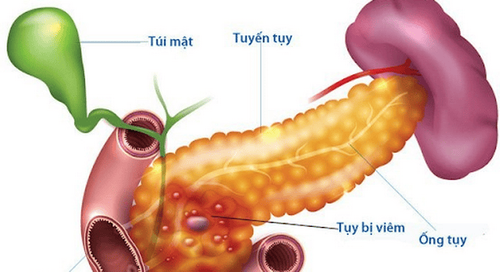
Sphincter of Oddi dysfunction (sphincter of Oddi disorder) is the term used to describe a heterogeneous group of pain syndromes caused by abnormalities in the sphincter's ability to contract. Disorders of the biliary and pancreatic sphincter of Oddi are classified as type I, II, or III, according to the Milwaukee classification. Sphincter of Oddi dysfunction appears to increase the risk of acute pancreatitis as well as the incidence of post-ERCP pancreatitis by more than 30%.
1. Common management when diagnosed with sphincter of Oddi
Various mechanisms have been recognised, but the exact role of sphincter of Oddi dysfunction in the pathophysiology of acute pancreatitis remains unknown. There is also an association between sphincter of Oddi disorder and chronic pancreatitis, but it is not clear whether this is a cause-and-effect relationship. Management of the sphincter of Oddi disorder is aimed at resection of the sphincter, usually endoscopic sphincterotomy (ES).
Patients with type I sphincter of Oddi disorder will benefit from endoscopic sphincterotomy in 55%-95% of cases. Sphincter of Oddi manometry is not necessary before endoscopic sphincterotomy in type I sphincter of Oddi disorders. For patients with types II and III, the benefit of endoscopic sphincterotomy is lower. These patients should be evaluated more thoroughly before performing laparoscopic sphincterotomy.
2. Disorders of the sphincter of Oddi may contribute to the risk of acute pancreatitis
Disorders of the sphincter of Oddi may contribute to the risk of acute pancreatitis by causing abnormal bile flow or pancreatic juice. In a study in Australian marsupials, whose pancreas and biliary anatomy are similar to those in humans, the combination of pancreatic ductal ligation and exocrine pancreatic stimulation with homogenous cholecystokinin/secrettin induced acute pancreatitis. . In another group, transmuscular flow was reduced by topical application of carbachol to the sphincter of Oddi, inducing pancreatic ductal pressures comparable to those of the pancreatic duct, in which the pancreatic duct was regulated. However, acute pancreatitis occurs only when carbachol is applied in combination with pancreatic secretion stimulation. Decompression of the pancreatic duct negated the effects. Therefore, the combination of pancreatic duct obstruction with exocrine hypersecretion is required to produce acute pancreatitis. Although this is a recognized complication of sphincter of Oddi disorder, this study demonstrated that sphincter of Oddi dysfunction may be a causative factor in the development of acute pancreatitis.
3. What do the studies say?
Kruszyna et al performed ERCP with sphincterotomy before and after sphincterotomy in a group of 30 patients with mild acute pancreatitis and compared the results with a control group of 30 patients with no evidence of stones. common bile duct or pancreatitis. Patients with pancreatitis had significantly increased common bile duct pressure, sphincter of Oddi pressure, and wave amplitude compared with controls. All parameters after sphincterotomy were significantly reduced. They concluded that sphincter of Oddi dysfunction, either primary or secondary to spasm due to gallstone migration through the canal, may have a role in acute biliary pancreatitis.
4. Disorders of the sphincter of Oddi leading to increased intrapancreatic duct pressure
Although there is little direct evidence for a role for the sphincter of Oddi in causing pancreatitis in humans, there is a great deal of circumstantial evidence. Fazel et al measured intrapancreatic duct pressure in 263 patients presenting with recurrent abdominal pain, recurrent acute pancreatitis, or chronic pancreatitis. Then, complete sphincterotomy was performed and sphincter of Oddi patients were found to have significantly higher pancreatic ductal pressures than those with normal sphincter of Oddi peristalsis. This difference was seen in all three groups (P < 0.01), and patients with acute and chronic pancreatitis did not have a significant increase in intraluminal pressure compared with those with abdominal pain alone. The authors concluded that disorders of the sphincter of Oddi lead to increased intrapancreatic duct pressure, but this increase in pressure is not the sole cause of pancreatitis.5. Abnormalities of the sphincter of Oddi implicated in the pathogenesis of acute pancreatitis of other etiologies
Organophosphate pesticides are a recognized cause of acute pancreatitis in humans. It acts by irreversibly inhibiting cholinesterase, resulting in delayed synaptic breakdown of acetylcholine and has been shown to induce pancreatitis in animals, possibly due to a combination of obstruction at the sphincter level of Oddi and cholinergic stimulation of pancreatic secretion. The scorpion venom causes the release of acetylcholine, which irritates the pancreas and sphincter of Oddi and causes pancreatitis in a manner similar to organophosphate poisoning.
Other rare causes of acute pancreatitis including hypercalcemia and hyperlipidemia may be related to abnormalities of the sphincter of Oddi function. High extracellular calcium stimulates smooth muscle and stimulates pancreatic secretion in animal models and it has been suggested that abnormal calcium regulation of the sphincter of Oddi may be an underlying factor in the pathophysiology. A study in hypercholesterolemic rabbits showed failure to relax the sphincter of Oddi back indirectly suggesting that sphincter of Oddi dysfunction may contribute to the risk of pancreatitis. Thus, although its exact role is not known, the evidence, taken together, suggests that the sphincter of Oddi is to some extent an important factor in the development of acute pancreatitis. , including pancreatitis which may have other causes.
6. Management of pancreatic sphincter of Oddi disorder
In pancreatic sphincter of Oddi disorders up to 88% of patients would benefit from sphincterotomy. As a result, there have been calls from several regions for the removal of the current classification system in favor of a holistic system that includes biliary and pancreatic types. Future work should aim to understand the underlying mechanisms of the relationship between sphincter of Oddi disorder and pancreatitis as well as to identify patient factors that will help predict benefit from endoscopic therapy.
There have been calls from several regions to request that the current classification system be phased out in favor of an overall system that includes both biliary and pancreatic types. Future work should aim to understand the underlying mechanisms of the relationship between sphincter of Oddi disorder and pancreatitis and to identify patient factors that will help predict benefit from endoscopic therapy. There have been calls from several regions to request that the current classification system be phased out in favor of an overall system that includes both biliary and pancreatic types. Future work should aim to understand the underlying mechanisms of the relationship between sphincter of Oddi disorder and pancreatitis and to identify patient factors that will help predict benefit from endoscopic therapy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
1. Toouli J, Roberts-Thomson IC, Dent J, Lee J. Sphincter of Oddi motility disorders in patients with idiopathic recurrent pancreatitis. Br J Surg. 1985; 72 :859–863. [PubMed] [Google Scholar]
2. Varadarajulu S, Hawes R. Key issues in sphincter of Oddi dysfunction. Gastrointest Endosc Clin N Am. 2003; 13:671–694. [PubMed] [Google Scholar]
3. Petersen BT. An evidence-based review of sphincter of Oddi dysfunction: part I, presentations with "objective" biliary findings (types I and II) Gastrointest Endosc. 2004; 59 :525–534. [PubMed] [Google Scholar]