This is an automatically translated article.
Article written by MSc Mai Vien Phuong - Gastroenterologist, Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
The current “gold standard” test for esophageal cancer is endoscopic imaging and confirmed by biopsy. There are several barriers to endoscopy as a clinical tool to monitor patients at high risk for esophageal cancer, including cost, highly invested personnel, and invasive nature. encroachment of the procedure. The article below highlights new insights into the development and clinical validation of respiratory and circulatory biomarkers of esophageal cancer.
1.Diagnostic significance of esophageal cancer Esophageal cancer is the 6th leading cause of cancer death worldwide. Histologically, it is classified into 2 subtypes, squamous cell carcinoma and adenocarcinoma, each with a specific cellular origin, pathogenesis, and epidemiology.
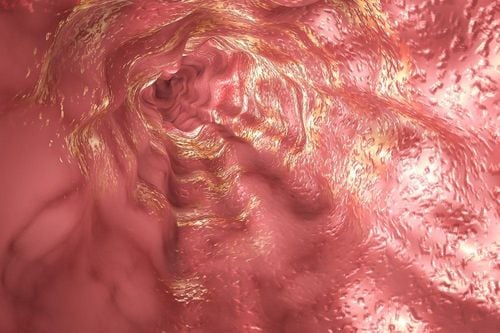
The current gold standard techniques for detecting and diagnosing esophageal cancer are endoscopic and biopsy is invasive. Furthermore, due to the absence of symptoms at an earlier stage of the disease, presentation and diagnosis are often late, resulting in a poor prognosis and 5-year survival rates as low as 15%.
Early diagnosis is associated with a much higher 5-year survival rate, and when limited to mucosal disease, specific survival rates of up to 98% have been reported. Better diagnostic methods are needed to move the majority of diagnoses to the earliest stages, and the expansion of access to routine endoscopy and wider use in the context of screening is not clinically effective. cost.
2. Current Diagnostic Methods of Esophageal Cancer The diagnosis of esophageal cancer and its premalignant lesions is currently limited to endoscopy and subsequent biopsy analysis. Endoscopy is a highly invasive and expensive diagnostic procedure and the current gold standard diagnostic technique for esophageal cancer and its precancerous lesions.
Standard white light endoscopy is limited in its scope, limited to the identification of macroscopic abnormalities that may indicate cancer, such as nodules and ulcers, and therefore cannot be identified. Early lesions appear to be grossly normal. While Barrett's esophagus is visible endoscopically, dysplasia in the Barrett segment is more difficult to identify because the lesions are often flat and difficult to distinguish from the surrounding non-dysplastic columnar epithelium.
Dysplasia classification is subjective and studies have shown that distinctions between dysplasia types vary widely among pathologists, leading to misdiagnosis and unnecessary interventional procedures. Likewise, random biopsy procedures are prone to sampling errors, adding to the potential for misdiagnosis.
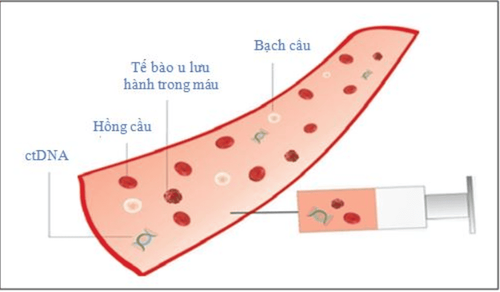
3. Urgent biomarkers of esophageal cancer Minimal and noninvasive biomarkers, mainly in blood and breath, represent the most likely candidates for facilitating Early detection of esophageal cancer.
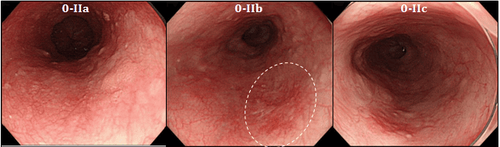
Ung thư thực quản giai đoạn sớm được nhìn thấy qua nội soi
Several candidate biomarkers for esophageal cancer have been proposed. However, their translation into clinical use has been slow. Biomarkers can be broadly defined as quantifiable parameters that differentiate normal processes from pathological ones with applications for diagnosis, prognosis, and treatment adjustment of patients.
The development of powerful, minimally invasive, cost-effective biomarkers for early cancer will change current diagnostic, prognostic and surveillance models, and may open up population screening capabilities.
Dấu ấn sinh học ngày càng được sử dụng nhiều trong chẩn đoán bệnh ung thư
3.1 Blood Biomarkers Autoantibodies have attracted interest as serological markers for esophageal cancer, due to their stability and persistence in serum samples. With improvements in antibody detection technology raising the detection limit, there is increasing interest in the use of autoantibodies as diagnostic and prognostic biomarkers for esophageal cancer.
Perhaps the most comprehensively studied is the tumor suppressor gene, TP53. The protein product of TP53 is a nuclear phosphoprotein and in normal human plasma, TP53 protein and anti-p53 antibodies are absent. The p53 mutation can cause the accumulation of non-functional proteins with increased stability and longer half-lives compared with native proteins. Anti-p53 production has subsequently been detected in the tissues, blood, and other body fluids of several types of cancer, including esophageal cancer. A meta-analysis by Zhang et al summarizing the diagnostic value of anti-p53 for esophageal cancer found that esophageal cancer patients had a seven-fold increased risk of plasma anti-p53 positivity. compared with the control group without cancer. However, despite its high specificity, the authors reported low sensitivity, suggesting limited clinical application.
3.2 The role of miRNA strand miRNA is a single-stranded, non-coding RNA that can regulate the expression of genes and proteins. miRNAs are highly expressed in stable form, with high inter-individual consistency in a variety of extracellular fluids including serum and plasma, and have attracted attention as biomarkers for cancer. mail and illness.
>>> Blood miRNA sequence test - new biomarker in diagnosis of esophageal cancer
Recent studies have reported circulating miRNAs in plasma/serum as diagnostic and prognostic markers potential in several gastrointestinal cancers - esophagitis, esophageal, gastric and colorectal adenocarcinomas. Although still an emerging area of research, recent meta-analyses have highlighted the potential of circulating miRNAs in the detection of esophageal cancer.
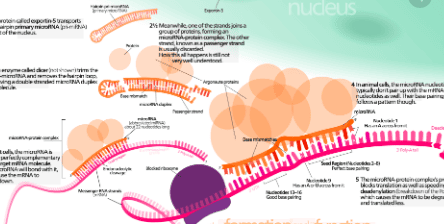
Sợi đơn miRNA sẽ là dấu ấn triển vọng trong chẩn đoán ung thư thực quản
4. The role of breath biomarkers Breath analysis represents an attractive way to detect cancer early, as it is completely non-invasive and relatively inexpensive compared to conventional methods. and provide quick results after sample collection. Breathable volatile organic compounds (VOCs) as biomarkers of disease have been recognized since the time of Hippocrates of Ancient Greece, who described fetal and fetal liver in his treatise on bad breath and sickness.
It is now known that a human breath is a complex gaseous mixture of more than 2000 unique VOCs, representing a reservoir of potential cancer biomarkers. Breath VOCs have shown clinical utility as possible biomarkers for lung, breast, prostate, colorectal, gastric and, more recently, esophageal cancers.
Many studies have shown that breath alkanes are associated with cancer, perhaps as a biological product of the oxidative stress pathway. Breath ethane was previously studied in end-stage esophageal squamous cell carcinoma and adenocarcinoma, with no difference compared with healthy controls.
More advanced technologies have been used to characterize VOCs associated with esophageal cancer. Head-space analysis of gastric contents urine from esophageal cancer patients using selected ion-flow tube mass spectrometry identified a number of VOCs that were differentially regulated compared with healthy controls. However, there is no dominant group of VOCs in the cancer group.
5. Breath test - New means of diagnosing esophageal cancer The first breath analysis study to determine breath VOCs in esophageal cancer identified a dominant expression pattern of phenol, with phenol, methyl phenol, ethyl phenol and hexanoic acid were significantly increased in esophageal cancer compared with healthy controls. In the most comprehensive study to date, Kumar et al investigated breath VOCs in esophageal squamous cell carcinoma, esophageal adenocarcinoma, Barrett's esophagus, and benign and cancerous conditions. gastric adenocarcinoma, compared with healthy controls. A total of 12 VOCs, including phenols, aldehydes, and fatty acids, were identified as discriminating against esophageal cancer and gastric cancer compared with a normal upper gastrointestinal (GI) tract.

Test hơi thở được sử dụng trong chẩn đoán ung thư thực quản
Furthermore, the model correctly distinguished esophageal adenocarcinoma from noncancerous controls (benign condition, Barrett metaplasia, and normal upper gastrointestinal tract), with sensitivity and specificity. The difference is 87.5% and 82.9%, respectively. Interestingly, no difference in VOCs was detected between early- and late-stage cancers, or between tumor size and VOCs concentrations.
6. Role of Mass Spectrometry - Proton Transfer Response Mass spectrometry - proton transfer reaction was recently used to determine breath VOCs in a small study of patients with Chinese esophageal cancer Country.
>>> The role of mass spectrometry-proton transfer reaction in the diagnosis of esophageal cancer (Part 1)
>>> The role of mass spectrometry-proton transfer reaction in the diagnosis of esophageal cancer (Section 2)
Although the study did not distinguish between esophageal squamous cell carcinoma and esophageal adenocarcinoma, the authors reported 20 ion peaks in the full mass spectrometry that were significantly different in cancer patients compared with healthy controls. Using stepwise discriminant analysis, the authors identified 7 ions with high discriminatory potential for esophageal cancer.
In contrast, with the study of Kumar et al., the authors also suggest that their predictive model distinguishes between early and late-stage cancers. However, these interpretations should be carefully balanced with the small number of participants used in the study.
7. Conclusion Recent advances have been made in the development and validation of new minimal and non-invasive biomarkers for esophageal cancer. Although several new serological markers have been investigated, they have not yet been translated into use as tools in clinical practice.
The recently developed field of breath and gas analysis for cancer detection represents a completely non-invasive approach to early detection and continuous screening of people at risk.
With improvements in the sensitivity of VOC detection technology, it is possible that the pool of breath and odor biomarkers will increase significantly. Although there are relatively few studies investigating breath biomarkers in esophageal cancer, early predictive models have shown some promise. Moving forward in this rapidly growing field, it is important to use standard approaches to breath sample collection, to minimize research heterogeneity. Furthermore, there is little evidence to support the biological origin of VOCs.
Currently, screening for gastrointestinal cancer is a scientific and effective measure for early detection of gastrointestinal cancer (esophageal cancer, stomach cancer, colon cancer) and giving a treatment plan. best treatment. Currently, Vinmec International General Hospital has a cancer screening package of esophagus, stomach (esophagus - stomach - colon) combining clinical and paraclinical examination to bring the most accurate results possible. .
The package of screening and early detection of stomach cancer includes:
Gastroenterology Specialist Examination (with appointment). Endoscopy of the esophagus, stomach and duodenum (with NBI machine, with anesthesia) Gastroscopy with anesthesia (drugs) Gastroscopy with anesthesia (VTTH) Routine histopathological examination fixed, transferred , casting, cutting, dyeing...biopsy specimens
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Pakzad R , Mohammadian-Hafshejani A, Khosravi B, Soltani S, Pakzad I, Mohammadian M, Salehiniya H, Momenimovahed Z. The incidence and mortality of esophageal cancer and their relationship to development in Asia. Ann Transl Med . 2016; 4:29. [PubMed] [DOI] Bystricky B , Okines AF, Cunningham D. Optimal therapeutic strategies for resectable oesophageal or oesophagogastric junction cancer. Drugs . 2011; 71 :541-555. [PubMed] [DOI] Bandla S, Pennathur A, Luketich JD, Beer DG, Lin L, Bass AJ, Godfrey TE, Little VR. Comparative genomics of esophageal adenocarcinoma and squamous cell carcinoma. Ann Thorac Surg . 2012; 93 :101-1106. [PubMed] [DOI] Bird-Lieberman EL, Fitzgerald RC. Early diagnosis of oesophageal cancer. Br J Cancer . 2009; 101 :1-6. [PubMed] [DOI] Yentz S , Wang TD. Molecular imaging for guiding oncologic prognosis and therapy in esophageal adenocarcinoma. Hosp Pract (1995). 2011; 39 :97-106. [PubMed] [DOI] Jankowski J , Barr H, Wang K, Delaney B. Diagnosis and management of Barrett's oesophagus. BMJ . 2010; 341 :c4551. [PubMed] [DOI] Roger Yazbeck, Simone E Jaenisch, David I Watson. From blood to breath: New horizons for esophageal cancer biomarkers, World J Gastroenterol. Dec 14, 2016; 22(46): 10077-10083