This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
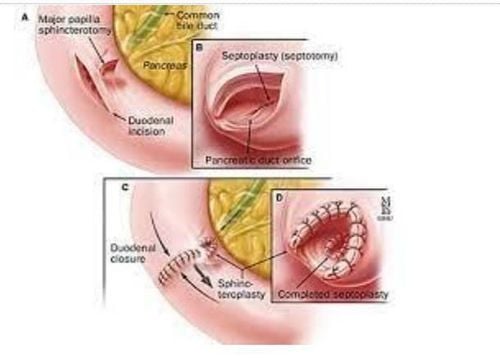
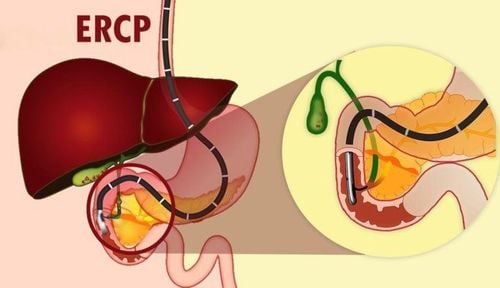
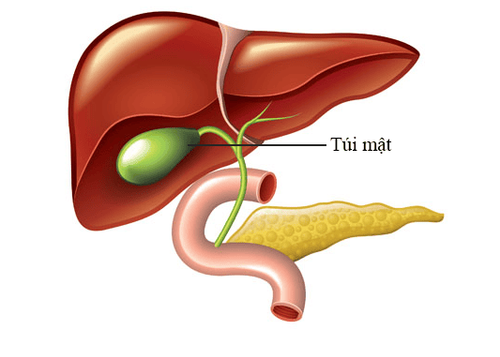
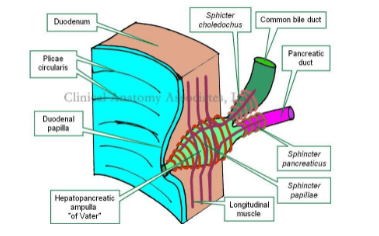
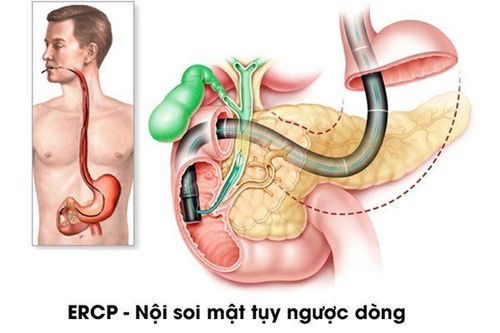
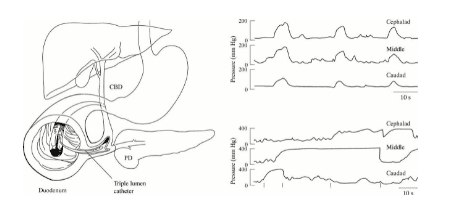
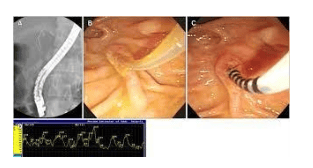
Sphincter of Oddi remains the gold standard for the diagnosis of sphincter of Oddi disorder. It is often combined with a diagnostic ERCP examination and includes manometer correction of the catheter. A three-tube catheter that allows continuous aspiration of pancreatic ductal fluid may reduce the risk of post-procedural pancreatitis.
1. Measure the pressure of the sphincter of Oddi
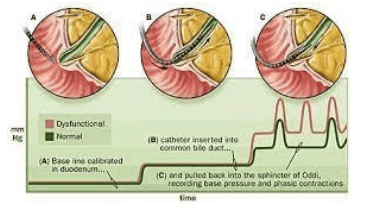
To determine which tube has been inserted, a small amount of contrast material is injected or some liquid is aspirated to determine its color. A “pull through” catheter is performed to assess the pressure profile and determine the location of the peak basal pressure. Normal basal sphincter pressure is approximately 15 mmHg but ranges from 3 to 35 mmHg. It is generally accepted that a baseline pressure greater than 40 mmHg (based on a threshold of 3 standard deviations above the mean) is abnormal. In patients with sphincter of Oddi stenosis, this recording is reproducible and unresponsive to muscle relaxants. In contrast, sphincter of Oddi dyskinesia is characterized by response to smooth muscle relaxants, excessive retrograde contractions (>50%), tachycardia (tachycardia rate >7/min), and contractile response Paradoxical squeeze of the sphincter of Oddi after intravenous administration. CCK dose.
2. Types of results for measuring sphincter pressure of Oddi type I
In sphincter of Oddi type I disorder, the sphincter of Oddi will be abnormal in 75%-95%. However, the frequency of abnormal biliary manometers varied from 28% to 60% for type II patients and from 7 to 55% in class III patients. Various factors may explain the difference in frequency of sphincter of Oddi disorders in published reports. For example, selecting patients with typical biliary or pancreatic pain over nonspecific pain would increase abnormal basal pressure output. sphincter of Oddi measures “snapshots” of sphincter pressure over the study period, which are not always reproducible.
A study of 12 patients with previously normal sphincter of Oddi showed evidence of elevated sphincter of Oddi pressure in 5 (42%) when retested after a median of 337 days. In addition, the pressures in the pancreatic and biliary tracts of the sphincter of Oddi may differ, so that evaluation of only one sphincter component, rather than both, will reduce the frequency of detection of sphincter of Oddi disorders. Current data suggest a discord rate between 35% and 65%. Therefore, both parts of the sphincter of Oddi need to be measured separately for a complete evaluation. This requires individual patient classification in relation to the pancreatic and biliary components of the sphincter of Oddi and is one of the reasons some experts call for a single holistic classification system. When both sides of the sphincter were evaluated, there was little difference between them in predicting abnormal background pressures.
3. Alternative endoscopic sphincter of Oddi manometry
Because sphincter of Oddi manometry is technically difficult, invasive, has variable diagnostic performance, and has recognized complications, other indirect methods of assessing sphincter of Oddi function have been developed. . These include the Morphine-Prostigmin stimulation test (the Nardi test; now obsolete), the ultrasound or MRCP-secrettin test, and the quantitative hepatobiliary scintigraphy. However, current data suggest that noninvasive tests have relatively low specificity and sensitivity, although there is some evidence that secrettin-stimulated MRCP may be useful in selecting Patients with suspected sphincter of Oddi disorder type II are more likely to benefit from sphincterotomy. Thus, despite the risks, and assuming careful patient selection, sphincterotomy remains the diagnostic tool of choice for most clinicians.
4.Acute pancreatitis after sphincter of Oddi
Acute pancreatitis is the main complication of sphincterotomy of Oddi . Increased pressure in the fallopian tubes, overfilling of the ductal system, dyscoagulation, and repeated pancreatic duct spasms and trauma are all considered etiological factors, possibly affecting the conduction of the ductus arteriosus. pancreatic duct. This hypothesis is supported indirectly by the observation that pancreatic ductal stenting after biliary sphincterotomy and needle sphincterotomy on pancreatic ductal stents was found to reduce the incidence of pancreatitis in patients with pancreatic ductal disorder. sphincter of Oddi.
5.Prevalence of pancreatitis after sphincter of Oddi
The rate of pancreatitis after sphincterotomy in patients with suspected sphincter of Oddi disorder has been found to be as high as 31%. Sherman et al found a much lower incidence of pancreatitis with suction catheters (1 of 33 patients; 4%) compared with infusion catheters (8 of 34 patients; 31%). However, Walters et al. found no difference in the incidence of pancreatitis when comparing the two manometer catheters (8% vs 13%). In a case series of 146 patients (207 sphincterotomy of Oddi measurements), Rolny et al reported a pancreatitis incidence of 6% using standard catheters. In addition, acute pancreatitis developed in 10 of 95 (11%) patients who had only pancreatometry, compared with 1 of 93 (1%) who had only densitometry.
6. Recommended methods to reduce the incidence of pancreatitis due to sphincterotomy of Oddi
Recommended approaches to reduce the incidence of pancreatitis due to sphincterotomy include assessment of the biliary sphincter of Oddi alone in patients with suspected biliary tract disease, limiting perfusion of the sphincter of Oddi to 1-2 minutes and select patients carefully.
For example, Scicchitano et al found a significantly higher incidence of pancreatitis when sphincterotomy of Oddi was indicated for idiopathic recurrent acute pancreatitis (acute recurrent idiopathic pancreatitis) compared with unexplained abdominal pain. (29% vs. 6%). The incidence of pancreatitis is 50% in patients with idiopathic recurrent acute pancreatitis and elevated sphincter of Oddi pressures. Temporary prophylactic pancreatic ductal stenting has been shown to reduce the incidence of pancreatitis in many patient groups, including those undergoing sphincterotomy of Oddi.
A retrospective review of 100 patients who underwent sphincterotomy of Oddi showed an overall incidence of pancreatitis of 17%. The incidence was significantly higher in patients who had undergone sphincterotomy and ERCP, compared with those who had only undergone sphincterotomy (26.1% vs 9.3%). Multiple regression analysis showed that sphincterotomy presents no additional risks other than those associated with ERCP. These results imply that other factors during ERCP, but not the manometer itself, lead to pancreatitis. The authors recommended that ERCP be performed at another session, possibly 24 hours after sphincterotomy of Oddi.
7. The risk of pancreatitis is intrinsic to the group of patients undergoing the procedure and the therapy provided, not the sphincterotomy of Oddi itself.
Results from other studies suggest that the risks of pancreatitis are intrinsic to the group of patients undergoing the procedure and the therapy provided, and not the sphincterotomy of Oddi itself. Freeman et al reported the complication rate of sphincterotomy in patients with suspected sphincter of Oddi disorder and in confirmed patients. Complication rates were 21% for patients who had undergone sphincterotomy and 25% when sphincterotomy was not performed prior to sphincterotomy.
Another study compared the incidence of ERCP-induced pancreatitis between patients with suspected sphincter of Oddi disorder, some of whom also underwent sphincterotomy, and a control group of patients with choledocholithiasis. . 27% of patients with suspected sphincterotomy developed pancreatitis after the procedure, compared with 3.2% of controls (P < 0.001). However, there was no significant difference in the incidence of acute pancreatitis in the first group between those with sphincterotomy of Oddi and those without (OR 0.72: 95% CI 0.08-9.2). . Similarly, in a large trial of 1000 patients undergoing ERCP with or without sphincterotomy of Oddi, Cheng et al found that sphincterotomy of Oddi was not a risk factor for post-ERCP pancreatitis.
Conclusion
Sphincter of Oddi manometry is essential in assessing sphincter function. Variation in complication rates between studies may be multifactorial and is related to the duration and duration of the procedure, the number of procedures performed with the manometer catheter, and the technique and skill of the operator. . However, it may be the case that in the experienced endoscopist, sphincter of Oddi resection does not significantly increase the risk of acute pancreatitis after ERCP and remains a useful tool in the diagnosis of sphincter of Oddi disorders. especially for types II and III.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.