This is an automatically translated article.
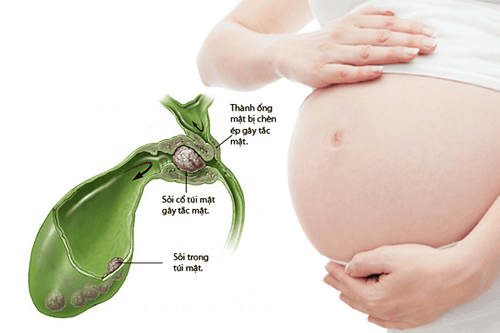
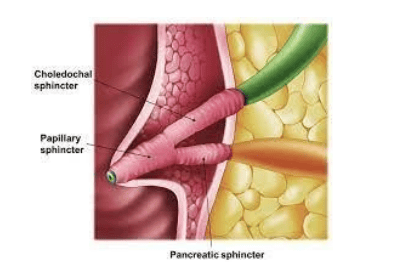
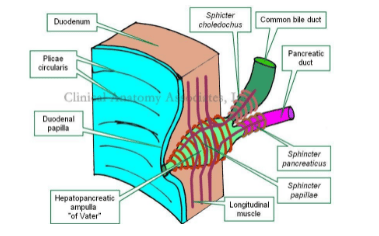
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalAcute pancreatitis is the main complication of sphincterotomy of Oddi. Increased pressure in the fallopian tubes, overfilling of the ductal system, dyscoagulation, and repeated pancreatic duct spasms and trauma are all considered etiological factors, possibly affecting the conduction of the ductus arteriosus. pancreatic duct.
1.Acute pancreatitis after sphincter of Oddi
The above hypothesis is supported indirectly by the observation that pancreatic ductal stenting after biliary sphincterotomy and needle sphincterotomy on pancreatic ductal stents was found to reduce the incidence of acute pancreatitis in patients sphincter of Oddi disorder.
The rate of pancreatitis after sphincterotomy in patients with suspected sphincter of Oddi disorder has been found to be as high as 31%.
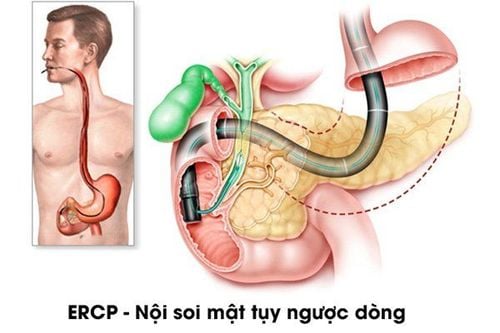
2.Acute pancreatitis after ERCP in patients with sphincter of Oddi
The overall incidence of pancreatitis after ERCP is commonly reported to be between 5%-15%. Prospective studies have consistently shown that disorders of the sphincter of Oddi increase the risk of post-ERCP pancreatitis (acute post-ERCP pancreatitis).
Cheng et al evaluated risk factors for acute ERCP-induced pancreatitis in 1115 patients who had undergone ERCP. Sphincter of Oddi disorder is suspected to be a significant risk factor with an OR of 2.6. In a prospective study of 1223 ERCP procedures, Vandervoort et al found that patients with measurable sphincter dysfunction of the sphincter of Oddi had a threefold increased risk of acute pancreatitis after ERCP (21, 7% versus 7.2%).
Freeman et al found an overall incidence of pancreatitis of 6.7% in the 1963 ERCP procedures with an odds ratio of 2.6 for suspected sphincter of Oddi disorder. A meta-analysis of 15 prospective clinical trials found that patients with suspected sphincter of Oddi disorder had a relative risk of developing pancreatitis of 4.09 (95% CI 3.37-4.96, P). <0.001). Therefore, sphincter of Oddi dysfunction is an independent risk factor for post-ERCP acute pancreatitis and the decision to proceed with ERCP, with or without sphincterotomy and/or sphincterotomy, should be made carefully. kidney.
Sphincterotomy for disorders of the sphincter of Oddi increases the risk of acute pancreatitis after ERCP. A small, although small, randomized controlled trial (n = 36), found a 33% incidence of pancreatitis after sphincterotomy in patients with sphincter of Oddi disorder without pancreatic ductal stenting. Five prospective randomized trials compared the incidence of acute pancreatitis after ERCP among high-risk patients with or without pancreatic ductal stenting. Four of these included patients with the sphincter of Oddi disorder. Of these four studies, there was a trend to reduce acute pancreatitis after ERCP with pancreatic ductal stenting, and two of them reached statistical significance. A meta-analysis of 5 prospective studies found a 3-fold increased risk of pancreatitis after ERCP without a pancreatic stent (15.5% vs 5.8%, OR 3.2, 95% CI 1). ,6-6.4).
3.The role of pancreatic stenting in the prevention of acute pancreatitis after ERCP
Results of randomized controlled trials including patients with sphincter of Oddi
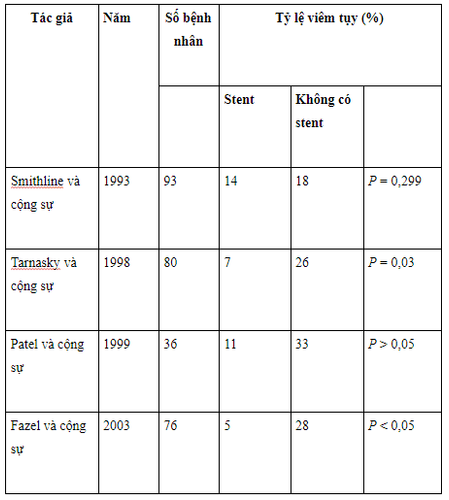
At least three case-control studies have also included patients with sphincter of Oddi disorder. Two of these significantly reduced acute pancreatitis after ERCP with pancreatic stenting, and in the other, the rate of pancreatitis decreased from 66.7% to 14.4% which was not completely significant (P=0.06). Therefore, there is substantial evidence that pancreatic stenting reduces the incidence of post-ERCP pancreatitis in high-risk groups such as sphincter of Oddi disorders. However, failure to successfully deploy stents can occur in 10% of patients, and failed pancreatic stenting can increase the incidence of acute pancreatitis after ERCP by sixteen-fold. Therefore, pancreatic stenting should not be attempted unless the probability of success is very high.
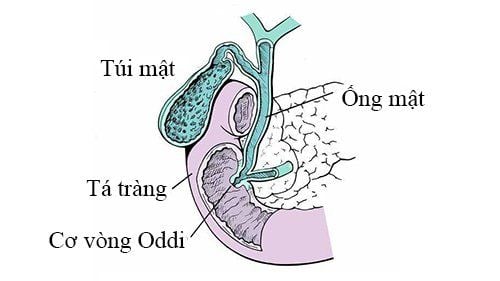
4. Sphincter of Oddi disorder and acute pancreatitis have been shown to be related
The relationship between sphincter of Oddi disorder and pancreatitis is a complex one. The association between sphincter of Oddi dysfunction and acute pancreatitis seems beyond doubt, especially given the unusually high frequency of sphincter of Oddi resection in idiopathic recurrent acute pancreatitis. Sphincter of Oddi disorders also significantly increase the risk of post-ERCP pancreatitis by more than 30%, although correct placement of pancreatic stents at the time of procedure appears to reduce this risk. However, although different mechanisms have been recognized, the exact role of sphincter of Oddi dysfunction in the pathophysiology of pancreatitis is unknown and it is unclear whether sphincter of Oddi dysfunction as a variable primary or secondary failure to other factors is the primary mechanism. There is also evidence linking the sphincter of Oddi disorder with chronic pancreatitis but whether this is a cause-and-effect relationship is unknown.
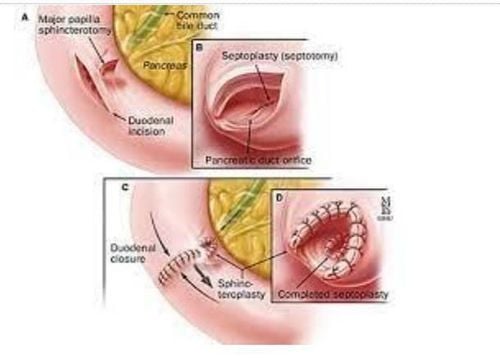
5. Sphincterotomy remains the management option for sphincter of Oddi
All patients with sphincter of Oddi disorder type I should undergo sphincterotomy and by general consensus this group does not require preprocedural manometry. The question of whether dual sphincter should be performed remains unanswered and further randomized trials are needed to clarify this. For patients with sphincter of Oddi disorder type II, studies have found that sphincterotomy is a useful guide in predicting response to sphincterotomy, although some studies are small. showed that barometric results were not correlated with clinical outcomes. However, most experts agree that patients with suspected sphincter of Oddi disorder type II should have the sphincter of Oddi removed before considering sphincterotomy.
6. Type III sphincter of Oddi disorder responds less well to endoscopic sphincterotomy
Management of patients with sphincter of Oddi disorder type III remains more challenging with response rates to sphincterotomy ranging from 8% to 65%. In general, sphincterotomy may be warranted if sphincterotomy is abnormal, but medical therapy should be attempted before manometry is performed. A detailed history is paramount for these patients. The more the pain pattern differs from the pattern outlined in the Rome II criteria, the less likely the patient is to benefit from treatment. Until a more appropriate method is available for characterizing patients with sphincter of Oddi type III, it will not be possible to conduct a randomized placebo-controlled trial of sphincterotomy. Ultimately, this will be the only way to demonstrate the benefit or alternative of sphincterotomy for presumptive patients with type III sphincter disorder of Oddi.
7. It is still best to measure both parts of the sphincter of Oddi to maximize the detection rate of the sphincter of Oddi disorder.
Recent evidence supports the need to measure both parts of the sphincter of Oddi to maximize the detection rate of sphincter of Oddi disorders. This dual classification has prompted calls for a single overall classification system from several regions. A recently published trial has also shown that other patient factors such as age, opioid use, delayed gastric emptying, and measurement of pancreatic pressure are more important predictors of response. response to double sphincterotomy compared with abnormal liver function tests and dilated ducts, on which the traditional classification system is heavily based. Larger prospective trials are required to identify other potential patient factors that may help predict response to therapy; these factors should be taken into account in any future overhaul to the current classification system.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.