This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
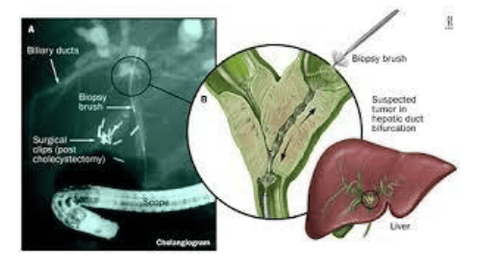
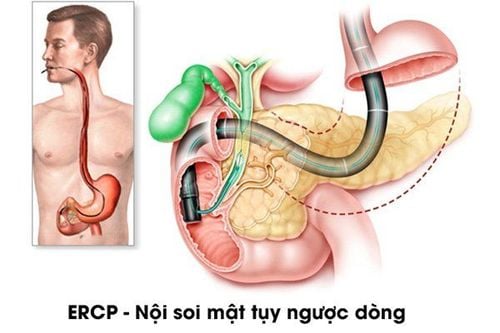
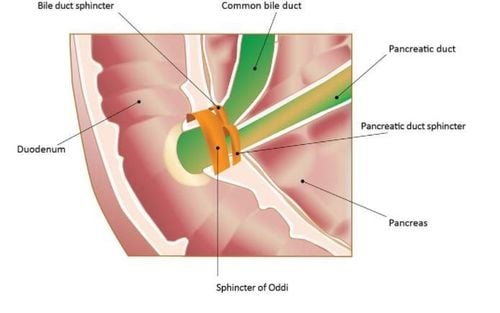
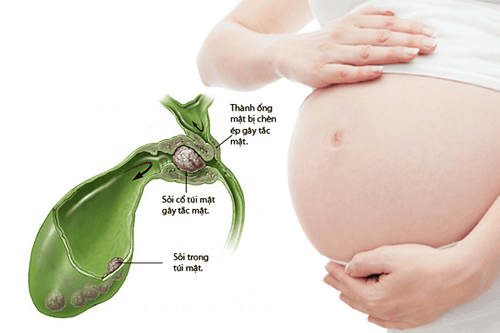
Endoscopic retrograde cholangiopancreatography is an endoscopic technique used to investigate and treat diseases of the biliary tract, pancreatic duct, and gallbladder. The bile ducts are the tubes that carry bile from the liver and gallbladder; The pancreatic duct carries pancreatic juice from the pancreas. Both of these tubes empty into the duodenum, the first part of the small intestine. So how is endoscopic retrograde cholangiopancreatography done and what should be paid attention to when bringing the bronchoscope to the ampulla of Vater?
1. Approach to a patient with jaundice before endoscopic retrograde cholangiopancreatography
A patient with jaundice, endoscopic examination must be performed with 2 purposes: establishing diagnosis and therapeutic solution. These goals cannot be accomplished using a straight bronchoscope, so endoscopic retrograde cholangiopancreatography should not be attempted in patients presenting with biliary obstruction or suspected obstruction unless the endoscopic physician has the ability to do so. perform drainage treatment. Therefore, an inexperienced endoscopic surgeon, or a person who has never performed a sphincterotomy or has not had a stent inserted, should not attempt endoscopic retrograde cholangiopancreatography unless he or she can suggest a course of treatment. reduce the pressure.
In the case of an inexperienced endoscope performing endoscopic retrograde cholangiopancreatography, a surgeon or radiologist must be available to provide immediate decompression therapy after endoscopic surgery. Identify evidence of obstruction. In some cases, although an experienced endoscopic surgeon may still fail to treat decompression, it is common for a person with minimal experience to perform the procedure for a specific purpose.
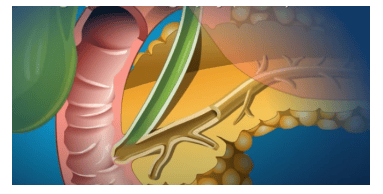
2.Advantages of endoscopic retrograde cholangiopancreatography compared with percutaneous cholangiography
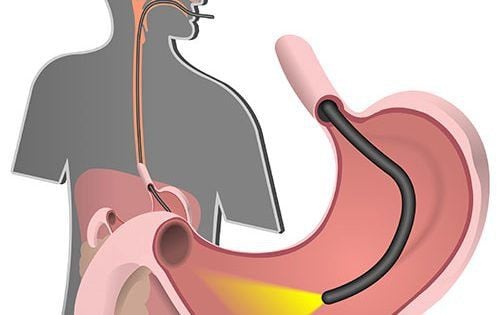
After passing the bronchoscope through the duodenum, the scope can be kept in a position to gain access to the Vater papilla. The main advantage of endoscopic retrograde cholangiopancreatography compared to percutaneous cholangiography is that it allows the mucosa of the upper gastrointestinal tract to be examined, thereby providing the necessary information regarding a variety of diseases and complex symptoms. complex, especially inflammatory and cancerous disease of Vater's papilla. The new generation duodenoscope with a wide viewing angle allows visualization of the end of the esophagus, and when the scope is controlled in the right position, it shows the pyloric lumen. Of course, the stomach needs to be thoroughly examined before the endoscope is inserted through the duodenum. The entire stomach, the gastro-oesophageal junction, should be examined as this provides some important pathological information. Observation of the gastro-oesophageal junction becomes clearer with the lateral bronchoscope thanks to the easy curvature of the tip so that lesions in the center-bulge area are not missed.
3. It is necessary to observe the stomach with a tiltingoscope during the process of bringing the bronchoscope to the ampulla of Vater
The stomach is considered an organ to be examined, not a tube through which the scope can reach the ampulla of Vater. Close observation during endoscopy can assess the physiological function of the gastrointestinal tract. Peristalsis visualization during endoscopy helps assess gastric function and can rule out inflammatory pathology and hard infiltration of the mucosa through the mucosa. Extrinsic pressure on the posterior wall of the stomach is a consistent important finding in relation to pancreatic disease, both malignant and benign. Pancreatic pseudocysts can press on the posterior wall of the stomach, narrowing the lumen and affecting the stomach's ability to contract. Evaluation of antrum function as well as flexibility and hardening is also important in examining the entire stomach for both inflammatory and malignancies. Hardening of the antrum is an important sign and must be watched for during endoscopy.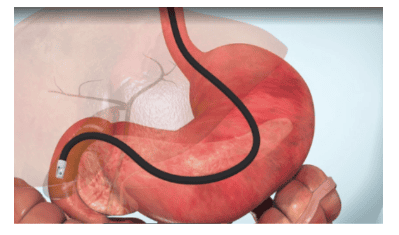
4. Identify the pylorus when inserting the bronchoscope to the D2 of the duodenum
The identified pylorus is usually located at the 6 o'clock position on the screen and the pylorus is observed closely before the laparoscope is passed. The duodenal wall is usually transiently visible, unless the bronchoscope stops to fully observe its wall. It is also important to note that with careful endoscopic examination, the pathological state of the duodenum can be determined, and it is found that about 10% of duodenal ulcers have lateral illumination (bilioscope- retrograde pancreas) was detected while the straight light endoscope was missed.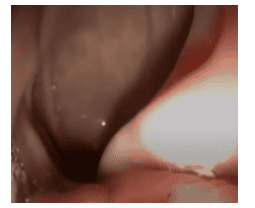
5. Diverticulosis around the duodenal papilla – common difficulties in endoscopic cholangiopancreatography
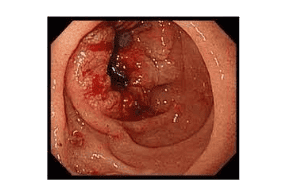
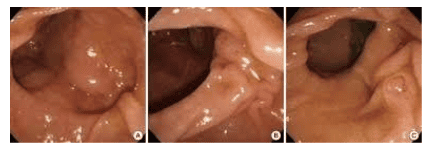
When reaching the ampulla of Vater, the endoscopist should always closely observe the periampullary structures. According to the authors, this is well done with a lateral light duodenoscope.
Duodenal diverticula were found to be closely associated with the large but uncommon papilla, Hughes & Kernult 1954 found this problem in 20% of their cases. Meanwhile, Dowby et al (1962) found that the diverticulum around the duodenal papilla accounts for 10%. Peripapillary diverticulum is often closely associated with the segment and OMC and pancreatic duct. Fortunately, they usually have wide necks (mouths). These diverticula themselves are asymptomatic, but if they are located adjacent to the large duodenal papilla, they will affect the hepatopancreatic ball, especially when the diverticulum is located above the ceiling of the duodenal papilla, making catheter placement difficult. this is a contributing factor to catheter failure) or perforation during endoscopic sphincterotomy).
6.It is necessary to determine the nature of the diverticulum and its relationship with the ampulla of Vater to facilitate the passage of the Vater papilla
Peripapillary diverticulum may be one, two, or three, posing the challenge of identifying the papilla and correctly orienting this structure for endoscopic access (catheterization). Several peripapillary images of Vater were obtained during endoscopic retrograde cholangiopancreatography showing the presence of a duodenal diverticulum in approximately 20%. For guidance and orientation purposes, the papilla was positioned on the wall of the diverticulum mouth. The papilla located in the diverticulum is a difficult site to locate a catheter in, especially when the papilla is located in the lower wall of the diverticulum. Evaluation of papillae in this setting can be difficult and requires principles of access to it, such that the bronchoscope should be in a short route, with the patient lying prone more easily able to identify the papilla and for biliary-pancreatic imaging. If more than one diverticulum is present, a short position bronchoscope (60-65 cm) allows identification of the diverticulum and the location of the papilla. The longitudinal fold will be visible towards the diverticulum, confirming that the papilla is located within that diverticulum. Furthermore, the papillae are almost never located in the diverticulum, usually located above the Vater papilla. One can use this property to identify the large papilla because sometimes when the papilla is not found it is necessary to rule out whether it is located in D1, D. or in the diverticulum. If a diverticulum is present, it will be located between the end of the diverticulum to the papilla.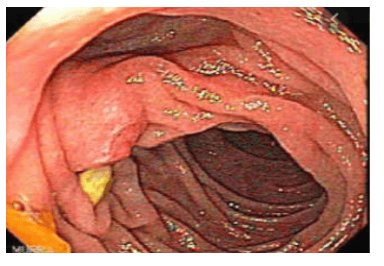
7. Sphincter dysfunction
Sphincter dysfunction caused by abnormal anatomical changes or changes associated with a parapapillary diverticulum. The presence of a foreign body (bezoar) can disrupt the drainage of the bile-pancreatic duct and can cause biliary colic and acute pancreatitis. If the papilla is located below the diverticulum adjacent to the diverticulum wall, similar dysfunction will occur. This phenomenon can be identified by carefully examining the papilla and studying its activity during peristalsis. Peristalsis can compress the diverticulum and eventually cause physiological dysfunction of the papillary muscle. Therefore, sphincterotomy can be performed to prevent this from occurring, especially if biliary tract dilatation is present and liver dysfunction is present.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.