This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Dysfunction of the gallbladder (GB) is a motility disorder caused primarily by metabolic abnormalities or by alterations in primary motility. Sphincter of Oddi (SO) dysfunction includes motility abnormalities of the biliary or pancreatic sphincter of Oddi.
1.Overview
Dysfunction of the gallbladder and/or biliary sphincter of Oddi produces similar pain patterns. Pain due to dysfunction of the pancreatic sphincter of Oddi may be similar to pain from acute pancreatitis. The symptom-based diagnostic criteria for gallbladder and biliary sphincter dysfunction are stable moderate to severe pain in the epigastrium and right upper quadrant of the abdomen that persists for a short period of time. at least 30 minutes. Gallbladder motility disturbance was suspected after excluding gallstones and other structural abnormalities.
2.Direction of diagnosis of gallbladder dysfunction and sphincter of Oddi
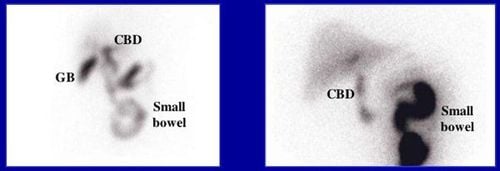
This diagnosis should then be confirmed by cholecystokinin-induced decrease in gallbladder ejection fraction on cholescintigraphy and after resolution of recurrent biliary pain after cholecystectomy. Symptoms of biliary sphincter of Oddi dysfunction may be accompanied by features of transient biliary obstruction, and symptoms of pancreatic sphincter of Oddi dysfunction are associated with elevated pancreatic enzymes and even pancreatitis.
Biliary sphincter of Oddi dysfunction is commonly observed in patients after cholecystectomy. The sphincter of Oddi measurement is valuable for selecting patients with sphincter dysfunction; however, due to the high complication rate, these patients should be referred to a specialist unit for evaluation. Therefore, invasive tests should be performed only when there is convincing clinical evidence and after noninvasive testing has shown negative results. The Committee recommended that biliary or pancreatic sphincter division be considered only when the patient has severe symptoms, the necessary criteria are met, and other diagnoses are excluded.
3.Pathophysiology of biliary tract and gallbladder
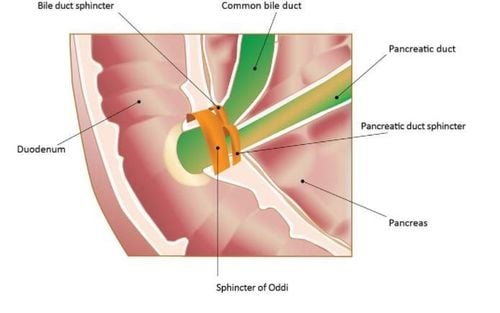
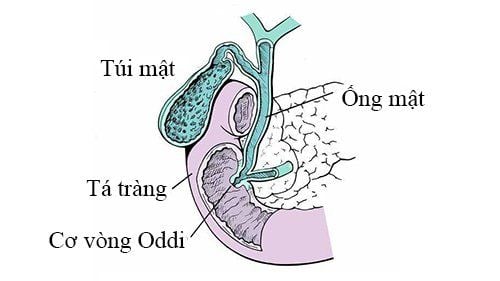
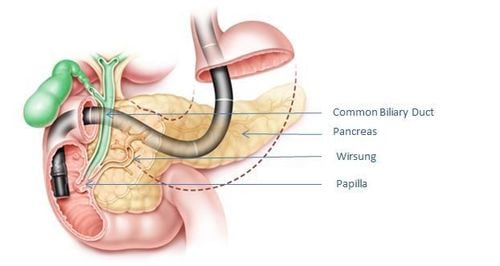
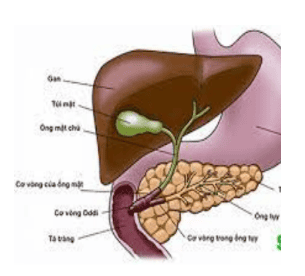
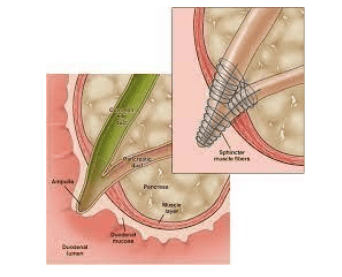
The biliary tract transports, stores, and regulates the continued excretion of bile in the liver. Bile is transported by intrahepatic and extrahepatic bile ducts and into the duodenum to contribute to the digestion and absorption of fats. During the congestive phase, resistance of the sphincter of Oddi.
These pressure changes create a gradient between the common bile duct and the gallbladder that redirects the flow of bile toward the gallbladder through the cystic duct. However, approximately 25% of hepatic bile enters the duodenum probably between physical contractions of the sphincter of Oddi.
It also occurs in the digestive and digestive tracts, where bile is continuously mobilized by pulsating and non-convulsive contractions in the gallbladder and through the cystic duct. The flow of bile through the cystic duct is complex, and some studies have shown that the flow through the cystic duct is bidirectional. Bidirectional flow through the cystic duct can best be explained by the gallbladder acting as a bellows that contract and relax intermittently.
During the digestive phase, real bile enters the duodenum due to gallbladder contraction and relaxation of the sphincter of Oddi preceded by sequential activation of enteric, antral, and enteric neuronal mechanisms. The sphincter of Oddi also plays an involved role in regulating the flow of pancreatic secretions into the duodenum. Alterations of any of these components may lead to intermittent abdominal pain, transient elevations of liver or pancreatic enzymes,
4. Gallbladder dysfunction and sphincter of Oddi are easily misdiagnosed with some other digestive diseases
Gallbladder and sphincter of Oddi dysfunction are relatively rare conditions, but their main clinical presentation, pain in the right upper quadrant and epigastric region, is not easily differentiated from those occurring occurs in common conditions such as gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), functional gastrointestinal disorders, gallstones, and high-risk complications from cholecystitis and cholecystitis. pancreatitis. In addition, sphincter of Oddi dysfunction itself may be responsible for abnormalities in the liver and pancreas. Therefore, these disorders need to be ruled out before a patient with suspected gallbladder and sphincter of Oddi dysfunction is referred for extensive investigation with invasive procedures and laparoscopic and surgical management. inappropriate technique.

5.Classification of gallbladder dysfunction and sphincter of Oddi
Current diagnostic criteria and guidelines for clinical evaluation and treatment have been developed taking into account specific aspects of gallbladder and sphincter of Oddi dysfunction, which are fundamentally different from those of other functional gastrointestinal disorders. Dysfunction of the gallbladder and sphincter of Oddi (type E) is classified as functional gallbladder disorder (E1), biliary sphincter of Oddi disorder (E2), and glandular dysfunction of the sphincter of Oddi. pancreas (E3). Compared with the previous Rome II criteria, the major change in the proposed criteria is to make them more stringent to reduce the number of unnecessary invasive procedures and surgical operations in patients with present upper abdominal pain.
Biliary and pancreatic pain should be defined by location, severity, mode of onset, duration, and absence of typical symptoms of GERD, functional dyspepsia, and IBS. The features of biliary and pancreatic pain in gallbladder and sphincter of Oddi dysfunction are not supported by any published evidence. They are based on similarities with the pain characteristics of patients with gallstones and patients with pancreatitis. It is also based on the consensus of the authors of this paper.
Therefore, these consensus-based symptom criteria should only be considered generalizations and not necessarily true in all patients. However, by excluding GERD, IBS, functional gastrointestinal disorders, and chronic abdominal pain, it will be possible to reduce unnecessary invasive procedures and surgical interventions. Psychosocial aspects appear to be associated with functional gastrointestinal disorders. These relationships may also occur in patients with dysfunction of the gallbladder and the sphincter of Oddi.
6.Classification of gallbladder and sphincter of Oddi dysfunction
Gallbladder and sphincter function of Oddi disorders
1. Gallbladder dysfunction
2. Functional biliary sphincter of Oddi disorders
3. Functional pancreatic sphincter of Oddi disorders
7. Should endoscopic retrograde cholangiopancreatography be used to diagnose patients with suspected gallbladder or sphincter of Oddi disorders in the first place?
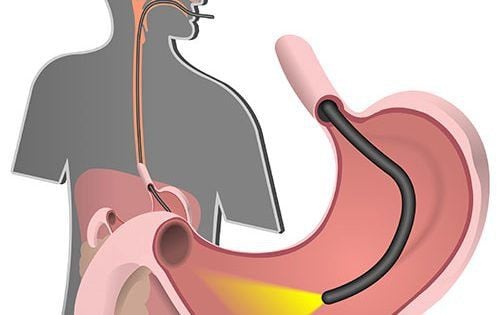
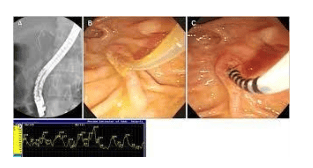
Patients with upper abdominal pain who do not meet the Rome III symptom-based criteria for gallbladder pain and functional sphincter of Oddi should not be indicated for endoscopic retrograde cholangiopancreatography (ERCP) or invasive procedures. other encroachment. Those who qualify for the Rome III criteria should be evaluated initially with noninvasive procedures and eventually with therapeutic trials that will most likely identify the majority of patients with pain of no origin. origin from the pancreas and therefore will not require further investigation. This approach will also select a small number of patients who may require more invasive procedures and who should be referred to centers dedicated to the study and treatment of pancreatic disorders with the device. appropriate and trained staff (see clinical evaluation).
Precautions to avoid unnecessary ERCPs as potential complications of this procedure, primarily pancreatitis, vary widely according to the endoscopist's experience and whether it is being performed for the purpose. diagnosis or treatment. In the literature, the incidence of posterior acute pancreatitis can be as high as 24%, and major complications and reported mortality vary from 1.4% to 1.8% and 0% to 0 respectively. .3% for diagnostic procedures, and 5.0% to 9.0% and 0.5% to 0.9%, respectively, for treatment procedures.
8. Diagnostic criteria for gallbladder disorders and sphincter of Oddi . function
Must include pain in the right epigastric and/or upper quadrant and all of the following:
Pains lasting 30 minutes or more Recurrent symptoms occurring at varying intervals (no (must be daily) Pain that gradually increases to a stable level Pain is moderate to severe enough to disrupt the patient's daily activities or lead to emergency department visits Pain that does not improve with bowel movements pain not relieved by position change Pain not relieved by antacids Rule out other structural disease that could explain symptoms Supporting criteria
Pain may present with one or more of the following features :
Pain accompanied by nausea and vomiting Pain spreading to the back and/or lower right side Pain waking up in the middle of the night Performing ERCP at Vinmec International General Hospital allows endoscopic diagnosis and treatment Under safe sedation, the patient is no longer afraid of endoscopy using the most modern technical equipment.
ERCP procedure performed at Vinmec using a modern flexible endoscope system, Endocut electric knife has the advantage of not causing pancreatitis, pancreatic reaction.
Especially, Vinmec has a team of leading prestigious doctors, well-trained with experience of over 1000 surgeries, specifically:
Master, Doctor Nguyen Ngoc Thang with 17 years of experience in the field of surgery Gastroenterology, hepatobiliary system, and over 09 years of experience in endoscopic interventions, especially the technique of endoscopic retrograde cholangiopancreatography (ERCP). Master, Doctor Duong Xuan Loc with more than 12 years of experience as a Gastroenterologist. The surgeons are all highly skilled people, making the surgical and postoperative process painless; Professional and dedicated patient care team.
Besides, at Vinmec, we always ensure to follow strict principles in sterilization and disinfection to prevent the spread of pathogens through endoscopes for patients and medical staff.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.