This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
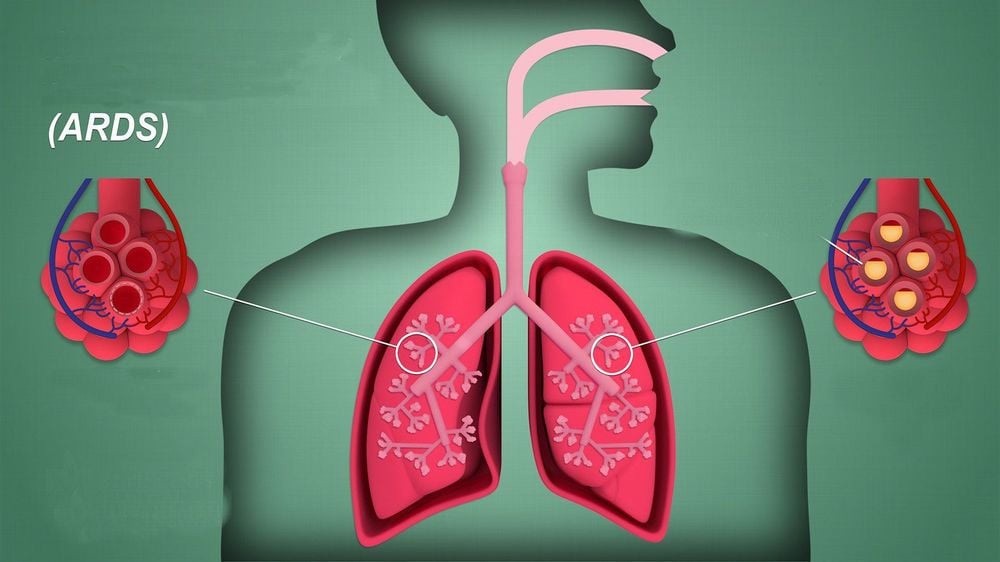
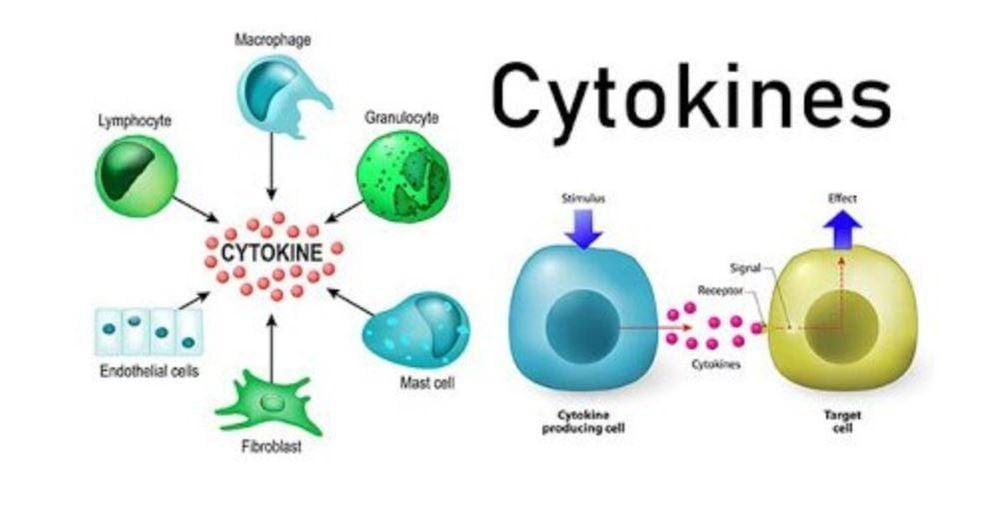
In the early stages of acute pancreatitis (AP), a large number of cytokines induced by localized pancreatitis severely compromise intestinal barrier function, intestinal bacteria and endotoxins enter the bloodstream , which causes an inflammatory storm, leading to multiple organ failure, infectious complications, and other disorders, and ultimately death.
Intestinal failure occurs early in the course of acute pancreatitis, promoting its development. As an alternative method to detect small intestinal bacterial overgrowth, the hydrogen breath test is safe, noninvasive and convenient, indirectly reflecting the gut microbiota counts in acute pancreatitis. next.
Maintaining intestinal barrier function and minimizing and preventing the migration of intestinal bacteria have become key to controlling the occurrence and development of severe acute pancreatitis. This reduces complications in the early stages of the disease. Multiple authors performed this study to investigate changes in gut microbiota and organ function in acute pancreatitis, and to explore the correlation between gut microbial overgrowth and muscle function. acute pancreatitis.
1.Changes in gut bacteria measured using a hydrogen breath test
A study was carried out with the aim of examining the changes in gut bacteria measured using hydrogen breath test in the early stages of acute pancreatitis to elucidate the relationship between gut bacteria and bacteria. bowel and acute lung injury/ARDS. Early clinical intervention and maintenance of intestinal barrier function will be very beneficial in controlling the development of severe acute pancreatitis. The authors retrospectively analyzed the data of 456 patients with acute pancreatitis who met the diagnostic criteria of the 2012 "Atlanta New Classification Consensus for Acute Pancreatitis" and those who were admitted to the intensive care unit (ICU) of the Department of Gastroenterology, Huyen Vu Hospital of the Capital Medical University from 2016 to 2019. A total of 152 patients were hospitalized with inflammatory response syndrome systemic or organ failure and may cooperate with a hydrogen breath test within 1 week of admission. According to the 2012 "New Atlanta Consensus Classification for Acute Pancreatitis" improved Marshall scoring criteria, 1 patient with circulatory failure, 2 patients with renal failure, 66 patients without organ failure, 83 patients with respiratory failure. Excluded 1 patient with circulatory failure and 2 patients with renal failure. A total of 149 patients were eventually included. General data including age, sex, body mass index (BMI), acute physiology and chronic health score (ACHE acute pancreatitis)-II, and inflammatory mediators were obtained. ten. In this study, the authors used a hydrogen breath test to detect changes in gut bacteria in the early stages of acute pancreatitis and demonstrate that there is a correlation between ARDS and bacterial overgrowth. enteric bacteria in the early stages of severe acute pancreatitis.
2.Respiration test with hydrogen lactose
The lactose hydrogen respiratory test is a semi-qualitative noninvasive test, originally designed to measure oral-caecal time; It is currently used for many diseases of the digestive system, such as lactose intolerance, irritable bowel syndrome, indigestion, and nonalcoholic fatty liver. The premise of the hydrogen breath test to detect intestinal bacterial overgrowth is that human metabolism does not produce hydrogen or methane. Methanogens are not bacteria, but archaea, mainly present in the colon, making up 10% of the total anaerobic organisms.
Since methane production requires hydrogen metabolism, hydrogen and methane concentrations can be detected simultaneously with a carbohydrate breath test. The lactulose hydrogen respiratory test involves oral administration of lactulose (non-absorbed sugar) to the cecum, fermentation with coliform bacteria to produce hydrogen and methane, absorption into the circulatory system, and then exhalation to detect concentrations. degree of hydrogen / methane in the breath; when breath hydrogen/methane concentrations exceed baseline, a diagnosis of intestinal bacterial overgrowth can be reached.
3. Principle of the hydrogen breath test method
After oral administration of lactulose (non-absorbable sugar), it reaches the cecum and is fermented with coliform bacteria to produce hydrogen and methane, which is absorbed into the circulatory system and exhaled through the lungs. When the hydrogen concentration in exhaled breath exceeds the basal level, it is diagnosed as intestinal bacterial overgrowth. In this study, a portable hydrogen gas detector was used to detect patients' expired hydrogen levels to diagnose intestinal bacterial overgrowth. Changes in exhaled hydrogen concentration may reflect the number of bacteria in the small intestine. The results of the above study showed that in 37 patients with severe acute pancreatitis with ARDS, the mean hydrogen production rate at admission was 1.15 ± 0.58, at 72 hours was 2.85 ± 4.79 and at 96 hours is 1.31 ± 0.71. In 28 patients with severe acute pancreatitis without ARDS, the mean rate of hydrogen production at admission was 2.39 ± 2.61, at 72 h was 1.68 ± 1.85 and at 96 h was 1.84 ± 1.86.
An increase in gut bacteria in patients with severe acute pancreatitis within 72 hours of admission is associated with the occurrence of ARDS. How to effectively maintain the stability of the intestinal barrier function in the early stages of the disease and prevent the intestinal bacterial overgrowth is an issue to be solved. Through this study, the author concluded that intestinal bacterial overgrowth in the early stages of severe acute pancreatitis is associated with ARDS. Furthermore, the occurrence of ARDS was associated with intestinal bacterial overgrowth within 72 h of admission. It has directional implications for maintaining intestinal barrier function in the early stages to reduce complications of early organ failure and late infection.
4. Gold standard for assessing intestinal bacterial overgrowth
The gold standard for the assessment of intestinal bacterial overgrowth is quantitative culture of duodenal or jejunal aspirates under aerobic and anaerobic conditions, and one study showed greater than 10 colony formations. 3 CFU/mL (colony forming units/mL). Due to the high cost and invasive nature of small intestinal fluid cultures, the hydrogen breath test, as an alternative to testing for intestinal bacterial overgrowth, has been proposed as an alternative. inexpensive, safe and non-invasive. It is widely used in the clinic as an important method for the diagnosis of intestinal bacterial overgrowth. However, the sensitivity range of the hydrogen breath test was 20%-90%, possibly due to the lack of uniform diagnostic criteria, which was resolved by the North American breath test consensus being recently announced.
5. Severe damage to the intestinal barrier function in the early stages of acute pancreatitis
In the early stages of acute pancreatitis, a large number of cytokines caused by localized pancreatitis severely disrupt the intestinal barrier function, leading to intestinal bacteria and endotoxins in the blood, causing inflammatory storm and lead to multi-organ failure. Hydrogen breath testing is currently being used for many digestive system diseases, such as lactose intolerance, irritable bowel syndrome, indigestion and nonalcoholic fatty liver. This test, as an alternative to detecting small bowel bacterial overgrowth (intestinal bacterial overgrowth), is used to indirectly reflect gut bacteria counts in inflammation. acute pancreas. This study aimed to examine the changes in gut bacteria measured using a hydrogen breath test in the early stages of acute pancreatitis to elucidate the relationship between gut bacteria and injury. acute lung injury (Acute lung injury) / acute respiratory distress syndrome (ARDS). Early clinical intervention and maintenance of intestinal barrier function will be very beneficial in controlling the development of severe acute pancreatitis (SAP).
6. Gut bacteria in patients with acute pancreatitis are different from those in healthy people
Clinical trials have shown that gut bacteria in patients with acute pancreatitis differ from gut bacteria in healthy individuals, and that the abundance of potentially pathogenic bacteria such as Enterobacteriaceae and Enterococcus was significantly increased while the The abundance of beneficial bacteria such as Bifidobacterium decreased significantly.
Animal experiments have shown not only to verify changes in gut bacteria in patients with acute pancreatitis, but also to correlate changes in gut bacteria and organ failure. However, neither of them showed a relationship between gut bacteria and organ failure in the early stages of acute pancreatitis. If we could understand the changes in gut bacteria using a hydrogen breath test in the early stages of acute pancreatitis, to understand the relationship between gut bacteria and acute lung injury/ ARDS, we can intervene and maintain intestinal barrier function as soon as possible, which will be very beneficial in controlling the development of severe acute pancreatitis.
7. Intestinal barrier dysfunction already present in the early stages of severe acute pancreatitis
As early as 2017, Zhang et al. and others used the qualitative standard of the hydrogen breath test to examine the relationship between severe acute pancreatitis and intestinal bacterial overgrowth. The results showed that intestinal barrier dysfunction was present in the early stages of severe acute pancreatitis; The rate of positive gut microbiota overgrowth is higher in patients with severe acute pancreatitis, and enteric bacterial overgrowth primarily occurs within 72 hours of onset. Finally, the authors found that there was a correlation between ARDS and intestinal bacterial overgrowth in the early stages of severe acute pancreatitis (P<0.05) consistent with the results of previous studies. this. Acute lung injury/ARDS is the earliest symptom of organ dysfunction in severe acute pancreatitis. In this study, it was concluded that the occurrence of ARDS was associated with intestinal bacterial overgrowth within 72 h of hospital admission. Studies have shown that severe acute pancreatitis intestinal failure occurs early, consistent with our study results.
Conclusion
Early organ failure in severe acute pancreatitis was found to be closely related to gut bacteria. Importantly, the study presented in this article also determined the timing of intestinal bacterial overgrowth, which has major guiding implications for the clinical management of acute pancreatitis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














