This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Acute pancreatitis is the most common serious complication following ERCP. Early recognition and appropriate management of potential adverse events are essential to reduce associated morbidity and mortality. In particular, the diagnosis of acute pancreatitis after late endoscopic retrograde cholangiopancreatitis can be fatal.
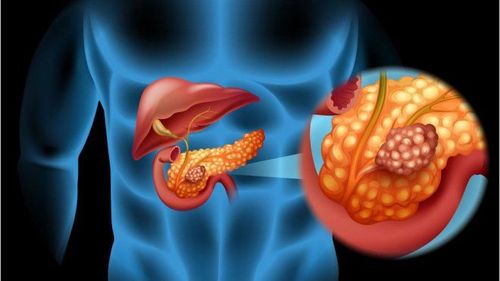
1.Diagnosing acute pancreatitis after endoscopic retrograde cholangiopancreatitis
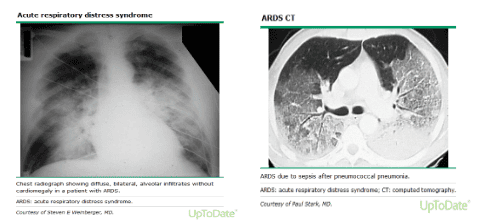
Most patients with acute pancreatitis after endoscopic retrograde cholangiopancreatitis have an acute onset of severe and persistent epigastric abdominal pain and, in about 50% of patients, pain radiating to the back. In about 90% of patients nausea and vomiting may persist for several hours. Patients with severe acute pancreatitis may have dyspnea due to diaphragmitis secondary to pancreatitis, pleural effusion, or acute respiratory distress syndrome, and 5% to 10% of patients with severe acute pancreatitis may have painless illness. and unexplained hypotension. To confirm the diagnosis, radiographic evidence with computed tomography may be needed, but biochemical tests are more commonly used, because they are inexpensive and sensitive. Early diagnosis of acute pancreatitis following endoscopic retrograde cholangiopancreatitis is important because late diagnosis can be fatal.
1.1. Pancreatic enzymes The diagnosis of acute pancreatitis following endoscopic retrograde cholangiopancreatitis can be complicated, as pancreatic enzyme elevations are common on examination, but are not generally associated with clinical pancreatitis.
There is no consensus in the literature about the ideal time after testing to claim serum amylase levels and what they really mean. Two prospective studies including 263 and 886 patients showed that 4-hour post-ERCP amylase levels were useful in predicting acute pancreatitis after endoscopic retrograde cholangiopancreatitis. The authors suggested that patients should fast for the next 12 hours and that amylase analysis should be ordered for all patients.
In patients with suspected pancreatitis, the degree and rate of pancreatic enzyme elevation may be a way to distinguish patients with acute pancreatitis after endoscopic retrograde cholangitis from those with pain from other causes. . Several studies have shown that patients with acute pancreatitis after endoscopic retrograde cholangiopancreatitis typically have serum amylase levels five times the upper limit of normal. The radiograph of the main pancreatic duct should be hospitalized if the 4-hour amylase level is greater than 2.5 times the upper reference limit. Patients who have not undergone a diagnostic procedure with pancreatic ductal contrast media should be hospitalized if the 4-hour amylase level is greater than five times the upper limit of normal. 4-hour post-ERCP amylase levels were useful in predicting acute pancreatitis after endoscopic retrograde cholangiopancreatitis in two prospective studies including 263 and 886 patients.
Bệnh nhân có nồng độ amylase huyết thanh cao hơn mức bình thưởng có thể là dấu hiệu viêm tụy cấp sau nội soi mật tụy ngược dòng
1.2. Differential diagnosis Not all patients with post-ERCP pain have pancreatitis. Other causes of abdominal pain after ERCP include air discomfort and perforation.
In patients with air pump discomfort, pain is generally not as severe as in acute pancreatitis after endoscopic retrograde cholangiopancreatitis and pancreatic enzyme levels may be normal or elevated, due to elevated pancreatic enzymes in the abdomen. most patients after ERCP. If serum lipase is less than three times the upper limit of normal, pancreatitis is unlikely (specificity 85 to 98%).
However, it should be noted that amylase and lipase begin to increase several hours after the onset of pancreatitis; therefore, blood tests performed immediately after ERCP may give false negative results. If clinical suspicion of pancreatitis is high, tests should be repeated at least 4-6 hours after ERCP.
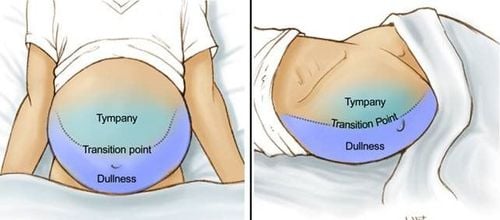
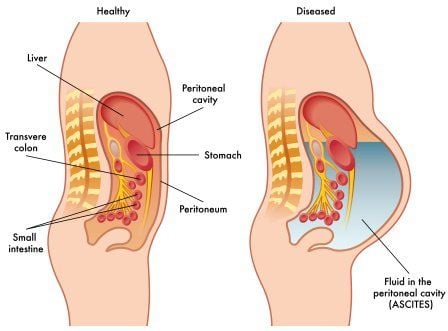
Patients with perforation after ERCP may have diffuse abdominal pain, abdominal distention, tachycardia, fever, and leukocytosis. Symptoms may appear shortly after the examination or several hours later. Many of the symptoms of perforation coincide with those of acute pancreatitis and if perforation is suspected, immediate abdominal computed tomography should be performed for intraperitoneal and retroperitoneal evaluation.
2. Treatment of acute pancreatitis after endoscopic retrograde cholangiopancreatitis
Most patients who develop acute pancreatitis after endoscopic retrograde cholangiopancreatography requiring hospitalization are classified as mild. In severe cases, admission to an intensive care unit may be necessary. Initial treatment should focus on the following:
Pain control
This often manifests as abdominal pain and should be one of the mainstays of treatment, as if left unchecked it can lead to hemodynamic instability. There is still controversy over the use of opioids such as morphine as it has been shown to increase pressure in the sphincter of Oddi, but there are no clinical data showing that this has resulted in worse pancreatitis. Indications for use: Meperidine, fentanyl, and morphine. Particular care should be taken in patients who are dehydrated or not receiving adequate fluids because hypovolemia and hemoconcentration can cause ischemic pain and increased lactic acidosis. Fluid replacement
Fluid replacement is one of the main items in the treatment of patients with acute pancreatitis after endoscopic retrograde cholangiopancreatitis. The use of crystalloid solutions, primarily Ringer Lactate, of 5 to 10 mL/kg/h is recommended in patients without restriction. In critically ill, hemodynamically unstable patients, 20 mL/kg over 30 minutes, then 3 mL/kg/h for the next 8 to 12 hours Care and monitoring
Because of the condition of these patients As this patient may deteriorate over the next 24 hours, they should be monitored for at least 48 hours. This monitoring includes vital signs, urine output, electrolytes, and blood glucose.
Antibiotics
Prophylactic antibiotics are not recommended in patients with acute pancreatitis after endoscopic retrograde cholangiopancreatitis, regardless of disease type or severity. Antibiotics should only be used for about 20% of patients with extrapancreatic infections. Nutrition
Fasting is recommended for all patients with acute pancreatitis after endoscopic retrograde cholangiopancreatography. The time to restart feeding depends on the severity of the pancreatitis.

Bệnh nhân Điều trị viêm tụy cấp sau nội soi mật tụy ngược dòng cần phải nhịn ăn
3. Prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatitis
Certain measures can reduce the incidence of acute pancreatitis after endoscopic retrograde cholangiopancreatography:
Adequate training and experience of endoscopists and assistants; Use guidewire techniques to access the biliary tract; Minimize the number of papillae passages; Prophylactic pancreatic stenting in patients at high risk for acute pancreatitis after endoscopic retrograde cholangiopancreatitis; Prophylactic pancreatic stenting in patients requiring guidewire placement in the pancreatic duct for biliary access (double guidewire technique); Selective bile duct catheterization if pancreatic ductal evaluation is not required; Minimize the volume of contrast injected into the pancreatic duct, if necessary; Careful use of combustion current during sphincter ablation; High-risk patients should undergo ERCP in specialized centers.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.