This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalProton pump inhibitor-responsive eosinophilia should be suspected if esophageal symptoms and eosinophil histological findings demonstrate a symptomatic and histological response to proton pump inhibitors.
Abbreviated terms:
EoE: Eosinophilic esophagitis: esinophilic esophagitis
GERD: Gastroesophageal reflux disease: Reflux esophagitis
IL: Interleukin: Interleukin factor
PPI: Proton pump inhibitor: Proton pump inhibitor Proton pump
PPI-REE: Proton pump inhibitor-responsive esophagal: Proton pump inhibitor-responsive esophagitis
Eosinophilia: eosinophils
VTQBCAT: eosinophilic esophagitis
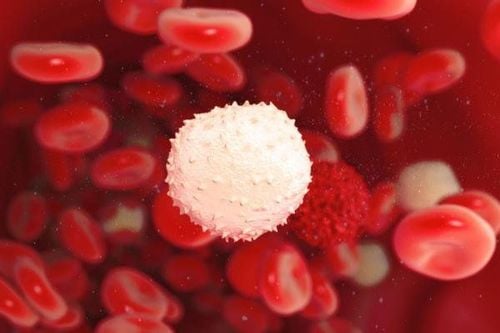
Eosinophils are One of the components of white blood cells produced by the bone marrow and one of the cells that promote inflammation, especially allergic inflammatory reactions. Therefore, large quantities of eosin can accumulate in tissues such as the esophagus, stomach, small intestine and sometimes in the blood when such individuals are exposed to the allergen.
Recommendations of the American Gastroenterology Association in 2013 emphasized that if increased BCAT is found in the esophagus, it should raise 3 possibilities: VTQTCAT, GERD and PPI-responsive esophageal BCAT (PPLREE).
1. Proton pump inhibitor-responsive eosinophilia (PPI-REE) and GERD
Eosinophils in response to proton pump inhibitors should be suspected if esophageal symptoms + eosinophilia histological findings demonstrate a symptomatic and histological response to proton pump inhibitors.Response to proton pump inhibitors (clinical, endoscopic and/or histologically) is not specific for GERD, therefore, additional evaluation for GERD (that is, pH testing) is recommended, according to standard clinical practice. standard. One-third of patients respond to treatment with proton pump inhibitors (PPIs); This group was identified as having PPI-responsive esophageal eosinophilia (PPI-REE).
In this article, we will present an overview of this newly discovered pathology process.
2. Overview of the pathology of eosinophilia in the esophagus
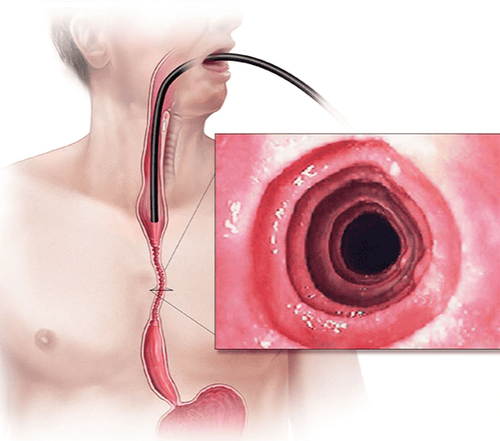
Eosinophilic esophagitis (abbreviated as EoE) is an emerging chronic esophageal disease, first described in 1993, with increasing incidence and prevalence in Western countries. During the 80s and early 90s, esophageal dense eosinophilia was mainly associated with gastroesophageal reflux disease (GERD). Over the next 15 years, EoE and GERD were treated as separate entities: Esophageal eosinophilia on exposure to high esophageal acidity when monitoring esophageal pH or in response to inhibitory therapy proton pump (PPI) is GERD, while normal or unresponsive pH monitoring to PPIs is EoE. Guidelines updated in 2011 described a new pathological phenotype, proton pump inhibitor-responsive esophageal eosinophilia (PPI-REE), referring to patients who appeared to have upper EoE clinical, but achieved complete remission after PPI treatment. Currently, PPI-REE must be formally excluded before EoE is diagnosed, as 30-40% of patients with suspected EoE are eventually diagnosed with PPI-REE. Intri eosinophils, the acid-suppressing capacity of PPI therapy, is becoming obsolete. There is increasing evidence that PPI-REE is genetically and phenotypically indistinguishable from EoE and that PPI therapy alone can completely reverse allergic inflammation. As such, PPI-REE may constitute a subtype of EoE and PPI therapy may be the first step of treatment and diet/steroid may represent advanced therapy. It is possible that the term PPI-REE will soon be replaced by a PPI-responsive EoE. The mechanism why some patients respond to PPI therapy (PPI-REE) while others do not (EoE), remains to be elucidated
3. Is esophageal eosinophilia a common disease?
Eosinophilic esophagitis (EoE) is a chronic, immunological/antigen-mediated esophagitis that is clinically characterized by symptoms associated with esophageal dysfunction and histology by eosinophilic predominance inflammation. Since its first description in the early 1990s, it has become an emerging cause of esophageal symptoms worldwide. Currently, it is the second most common cause of esophagitis after gastroesophageal reflux disease (GERD) and the leading cause of difficulty swallowing and food reactions in children and young adults. Furthermore, its incidence has steadily increased, and its prevalence has been consistently reported in Europe and the United States in 44 to 56 cases per 100,000 population, comparable to the prevalence of Crohn's disease in children in western countries.Rapid advances in the diagnosis and management of EoE have been completed over a period of seven years, as perfected by updated consensus guidelines in 2007, 2011 and 2013. One of the breakthroughs large is the description of a new underlying disease phenotype, which is a proton pump inhibitor-responsive esophageal eosinophilia (PPI-REE). This new phenotype refers to patients with symptoms and histological findings suggestive of EoE who achieve complete remission with PPI therapy. The PPI-REE classification has resulted in significant changes in the way the authors typically view and study esophageal eosinophils, as it differs from previous data suggesting the presence of eosinophils Intraepithelial oesophagitis is prognostic for GERD. Perspectives on PPI-REE continue to evolve from making a rigid distinction between GERD and EoE in 2007. More recent evidence suggests that PPI-REE and EoE may be closely related and that GERD may be a co-factor for EoE in some patients.
4. History of PPI-REE . pathology
1977-1992: Esophageal eosinophilia is almost universally believed to be the pathology of GERD.1977 and 1978: the first reports of eosinophil proliferation of the esophageal epithelium in two adults with dysphagia and no GERD symptoms were published. Several years later, isolated case reports further described similar conditions in adults and children. All of these case reports are attributed to a variant of eosinophilic gastroenteritis. However, during the 1980s and early 1990s, there were several reports of intraepithelial eosinophils in esophageal biopsies with GERD. Therefore, the incidence of esophageal eosinophilia is underappreciated because most pathologists consider the presence of esophageal eosinophils in the epithelium as pathological for GERD. In addition, esophageal biopsies are not a required standard of clinical practice in adult gastroenterology. In 1993, the first series of reports on EoE as a separate entity, included 11 adults with dysphagia, normal acidity on pH monitoring, and dense esophageal eosinophilia. (>20 eos/optical field) has been reported. Seven patients had hypersensitivity to certain foods and all necessary advanced interventional techniques (endoscopic balloon dilation and/or steroids in some cases) to resolve symptoms. The authors cautioned against a case of free esophageal eosinophilia for GERD.

Symptoms of esophageal dysfunction, mainly difficulty swallowing food; Esophageal eosinophilic infiltration (>15 eosinophils/field); There was no response to proton pump inhibitor (PPI) therapy or demonstrated normal exposure to esophageal acid on pH monitoring. Therefore, it has been suggested that a response to PPI therapy or increased acid exposure with pH monitoring is certain to have gastroesophageal reflux disease (GERD). The basic premise of this recommendation is that GERD, as a type of gastrointestinal acid disorder, responds to the acid-suppressing power of therapeutic PPIs. An illustrative example was provided in 2006 with the first case report of PPI-REE-like pathology in which two children and one adult with clinical, endoscopic and histological data suggesting EoE demonstrated complete lysis of esophageal eosinophils in response to PPI therapy. Interestingly, the authors conclude that: “while the presentation of these patients is highly suggestive of allergic esophagitis, their symptoms, and normalized esophageal tissue abnormalities after management are treated with PPIs, associated with acid reflux as the underlying cause”.
However, at the time, a number of forward-thinking authors raised the possibility that the rigid distinction between GERD and EoE based on PPI responsiveness might be too simplistic, based on underlying mechanisms. potential interaction between these disorders. In fact, the authors recommend a systematic trial of PPI therapy in all patients with the EoE phenotype (as we now have), suggesting that response to PPI therapy would not rule out the diagnosis. guess EoE. Between 2008 and 2010, several series of minor reports or case reports in children and adults also highlighted the existence of symptomatic patients who met clinical, internal and external criteria. bronchoscopy and histology for EoE with complete remission of clinical pathology with PPI treatment. In addition, there was no difference in treatment response rates when comparing topical steroid esomeprazole in adults with an EoE-based diagnosis of the presence of esophageal eosinophils.
2011: Description of PPI-REE as a new phenotype
In 2011, the first series of studies were reported evaluating the efficacy of PPI therapy in 35 patients with GI symptoms and true eosinophilia >15 eosinophils/field, 26 patients (75%) had clinical remission on PPI therapy, including remission in 50% of patients with the typical EoE phenotype (dysphagia). and/or disordered food response plus typical endoscopic findings). Patients with EoE and PPI-REE were indistinguishable at baseline by clinical, endoscopic, and histological features.
Monitoring pH of esophageal acid may or may not be elevated, questioning the ability of esophageal pH monitoring to differentiate between GERD and PPI-REE.
This new phenotype, PPI drug response to esophageal eosinophilia (PPI-REE), is recognized as one of the major advances in EoE research in the updated recommendations. 2011 consensus for the EoE.
2014: Pathological diagnosis of PPI-REE persists, possibly phenotype of EoE
Over the past three years, several large studies from the US and Europe have confirmed PPI-REE as a phenotype in number of patients with suspected EoE.
The prevalence of PPI-REE in these series ranges from 35% to 43%, underscoring its importance in clinical practice. As such, a PPI trial prior to arriving at a diagnosis of EoE is now mandatory to avoid unnecessary therapeutic interventions in PPI-REE, such as steroids or diet. This, as well as the difference between EoE and esophageal eosinophilia, is highlighted for the third time in recently published clinical reports.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesJavier Molina-Infante,David A. Katzka and Evan S. Dellon. Proton pump inhibitor-responsive esophageal eosinophilia: A historical perspective on a novel and evolving entity. Rev esp enfeRm dig(Madrid Vol. 107, No 1, pp. 29-36, 2015