This is an automatically translated article.
The article was written by Specialist Doctor II To Van Thai - Emergency Medicine Doctor, Emergency Department - Vinmec Hai Phong International General Hospital.Acute respiratory failure is defined as an acute decrease in the respiratory function of the respiratory apparatus and/or the gas exchange function of the lungs.
1. Severe acute respiratory distress syndrome
Acute respiratory failure is classified into three groups:
+ Respiratory failure due to hypoxemia when PaO2 is below 60mmHg when breathing room air
+ Respiratory failure due to hypercapnia when PaCO2 is above 50mmHg
+ Mixed respiratory failure when with both a decrease in PaO2 and an increase in PaCO2
Critical acute respiratory failure: A severe acute respiratory failure condition affecting many organs, threatening the patient's life. If not treated promptly and properly, the patient will die.
Causes of acute respiratory distress syndrome : All causes of acute respiratory failure can lead to acute respiratory distress syndrome, such as:
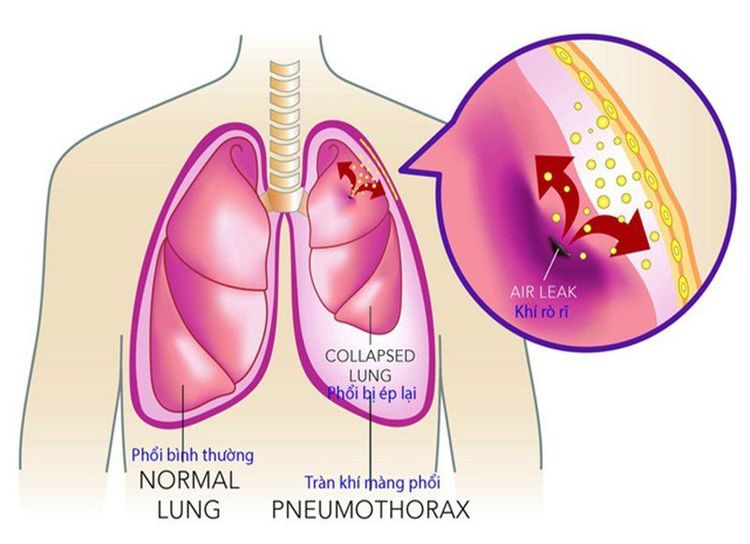
Central nervous system causes Systemic causes neuromuscular: Neuromuscular disease, drugs and poisoning, spinal cord injury, electrolyte disturbances, other causes: periodic paralysis, ... Causes from chest wall and diaphragm: Mobile rib array , multiple rib fractures Cause from pleural: Pneumothorax, pleural fluid Cause from lung parenchymal injury: Pneumonia, mechanical or blast wave lung injury, respiratory burn
Causes of the airways: Foreign body, bronchial asthma, edema or glottis spasm due to anaphylaxis, exacerbation of chronic obstructive pulmonary disease (COPD) Causes of pulmonary vascular disease: Pulmonary artery occlusion due to blood mass, gas, amniotic fluid,... Caused by other diseases: acute pulmonary edema due to heart failure, hyperthyroidism, convulsions, ... Assess severity of acute respiratory failure
2. Treatment of the cause of the acute respiratory distress syndrome
2.1. Bronchodilators (beta 2-adrenergic stimulants; anticholinergics)
Indicated for respiratory failure due to bronchospasm (COPD, bronchial asthma) Should be given by nebulizer first, if there is no response, then switch to intravenous infusion.
2.2. Corticosteroids
Indicated for exacerbations of bronchial asthma, COPD.
2.3. Antibiotic
When there are signs of infection (pneumonia, COPD exacerbation with evidence of infection).

2.4. Diuretic
Congestive heart failure, hemodynamic acute pulmonary edema, volume overload.
2.5. Treatment of surgical causes
Aspiration and drainage of fluid and air in the presence of effusion and pneumothorax. Movable rib array: fixed ribs by mechanical ventilation or fixed suspension. Cervical cord compression: surgical decompression.
2.6. Plasma exchange to remove antibodies in autoimmune diseases causing respiratory paralysis such as myasthenia gravis, Guillain-Barre syndrome
2.7. Some causes do not recover
amyotrophic lateral sclerosis, ...
3. Symptomatic treatment of acute respiratory distress syndrome
3.1. Principles of handling
Treatment of acute respiratory failure combined with treatment of the cause of respiratory failure.
3.2. Initial management and emergency transport
Quickly confirm the diagnosis of acute respiratory failure.
Rapid assessment of the causes of acute respiratory failure requiring immediate intervention: + Foreign body in the airway: Perform the Heimlich maneuver to remove the foreign body.
+ Pressure pneumothorax: Immediately insert a large needle into the intercostal space at the midclavicular line. Then transported to the hospital for pleural drainage and aspiration pneumothorax.
+ Apnea, respiratory paralysis: Squeeze ambu balloon and transport to hospital for endotracheal intubation.
Initial management of acute respiratory failure: + Open airway: remove foreign body, suction sputum.
+ The neck is flexed by the tests: push the forehead to lift the chin, raise the jaw.
+ Canuyn Grudel or Mayo against tongue drop.
+ Safe side-lying position if there is a risk of choking.
+ Squeeze the oxygen mask balloon to ensure ventilation.
+ Intubation with oxygen balloon (if possible).
Place a peripheral intravenous line. Transport the patient to the emergency and resuscitation center.
3.3. Treatment at the hospital
3.3.1. Emergency treatment
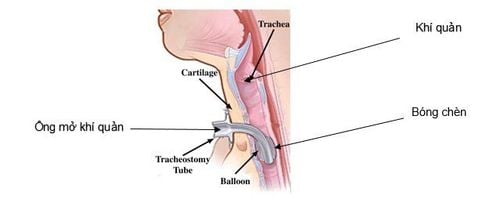
Bronchoscopy to remove airway foreign body. Open the pleura with a large tube to aspirate negative pressure pneumothorax. Indications for intubation: + Upper airway obstruction.
+ Loss of protective airway reflexes.
+ The ability to cough up sputum is greatly reduced or lost.
+ Severe hypoxemia does not respond to oxygen breathing.
+ Need for invasive artificial ventilation.
Ventilation control: Cases requiring ventilatory support + Hypoventilation:
Respiratory acidosis with pH < 7.25.
There is a risk that hypoventilation or hypoventilation will worsen: PaCO2 gradually increases; paralysis or fatigue of the diaphragm.
+ Severe hypoxia is poorly responsive to oxygen breathing.

3.3.2. Oxygen therapy
a) Principle: Must ensure blood oxygen (SpO2> 90%)
b) Breathing apparatus:
Nasal cannula: is a device with low oxygen flow of 1-5 l/min. Oxygen concentrations ranged from 24%-48%. Suitable for patients with moderate respiratory distress, patients with COPD or other causes of respiratory failure without shunts or low intrapulmonary shunts. Oxygen mask: is a low flow device 5-10 l/min. Oxygen concentration ranges from 35% to 60%. Suitable for patients with moderate respiratory failure due to damage to the alveolar capillary membrane (ALI, ARDS). Use with caution in patients with vomiting due to the increased risk of aspiration of vomit into the lungs. Non-rebreathing mask: a low-oxygen flow device of 8-15 l/min. High oxygen concentrations range as high as 60%-100% depending on the patient's flow needs and mask tightness. Suitable for patients with severe respiratory failure due to damage to the alveolar capillary membrane (pulmonary edema, ALI/ARDS). Use with caution in patients with vomiting due to the increased risk of aspiration of vomit into the lungs. Venturi mask: is a high-flow oxygen generator that can meet the needs of the patient's current. Oxygen concentration ranges from 24% to 50%. The advantage is for patients who need precise oxygen levels

3.3.3. Artificial Ventilation (TKNT)
a) Positive pressure non-invasive artificial ventilation: support ventilation for the patient through a mask (nose, nose and mouth)
Indications: + Respiratory failure due to hemodynamic acute pulmonary edema, exacerbation of COPD and asthma.
+ Severe respiratory failure with signs of muscle fatigue: exertion and respiratory rate above 30/min.
+ Acute respiratory acidosis (pH < 7.25-7.30).
+ Blood oxygenation status worsens (ratio PaO2/FiO2 < 200).
Contraindications: + Stop breathing.
+ Unstable hemodynamic status (uncontrolled hypotension or myocardial infarction).
+ Loss of airway protection.
+ Excessive phlegm.
+ Struggling or not cooperating.
+ The patient's condition does not allow the mask to be placed or the mask's tightness is not guaranteed.
b) Invasive artificial ventilation: when non-invasive ventilation is contraindicated or failed.

3.3.4. Treat the cause
a) Bronchodilators (beta 2-adrenergic stimulants; anticholinergics)
- Indicated for respiratory failure due to bronchospasm (COPD, bronchial asthma)
- Inhalation should be preferred first , if no response, switch to intravenous infusion.
b) Corticosteroids: indicated for exacerbations of bronchial asthma, COPD.
c) Antibiotics: when there are signs of infection (pneumonia, exacerbation of COPD with evidence of infection).
d) Diuretics: congestive heart failure, hemodynamic acute pulmonary edema, volume overload.
e) Drainage of fluid and air in the presence of effusion and pneumothorax.
f) Plasma exchange to remove antibodies in autoimmune diseases causing respiratory paralysis such as myasthenia gravis, Guillain-Barre syndrome.
g) Treatment of surgical causes:
- Movable ribs: fix the ribs by mechanical ventilation or fixation.
- Compression of cervical spinal cord: decompression surgery.
h) Some irreversible causes: amyotrophic lateral sclerosis, ...
4. Other treatments
Give fluids if not enough Vasoactive when enough fluids Treat cardiac arrhythmias Electrolyte balance Treatment of acidosis: Respiratory acidosis and metabolic acidosis Sedation during mechanical ventilation Ventilating position International General Hospital Vinmec is one of the hospitals that not only ensures professional quality with a team of leading doctors and nurses, a system of modern equipment and technology, but also stands out for its comprehensive medical examination, consultation and treatment services. professional; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
If you notice any unusual health problems, you should visit and consult with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.