This is an automatically translated article.
This article is expertly consulted by Master, Doctor Nguyen Le Duc Hoang - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital.Percutaneous tracheostomy for asphyxia is a technique that establishes an artificial airway between the surface of the neck and the trachea in the patient's neck. This is a procedure that brings many benefits to patients being treated in the intensive care unit.
1. What is percutaneous tracheostomy?
Percutaneous tracheostomy is a procedure that creates an artificial airway between the surface of the neck and the cervical trachea. Percutaneous tracheostomy has many advantages over surgical methods being applied to patients in the intensive care units.In patients undergoing percutaneous tracheostomy, the incidence of bleeding and wound infection is lower. In addition, because percutaneous tracheostomy is commonly performed in ICUs, the risks of complications associated with the transport of critically ill patients are reduced.
Vị trí mở khí quản qua da
2. Indications/contraindications for percutaneous tracheostomy
2.1 IndicationCases of upper respiratory tract obstruction. In the case of upper airway obstruction due to tumor, surgical approach to tracheostomy will be more appropriate; Long-term mechanical ventilation is required in cases of severe pneumonia, severe traumatic brain injury, multi-organ failure,...; Requires repeated sputum suction and other airway care; Treatment of obstructive sleep apnea unresponsive or intolerant to CAP. 2.2 Contraindications
Absolute contraindications
Difficult to determine neck anatomy; Have a history of radiation therapy or neck surgery; Clearing the airway in an emergency; Skin and soft tissue infections requiring surgery; Uncorrected pathology of coagulopathy; Patients with hypotension or hypovolemia; There is a disease causing neck deformity: Tumor, enlarged thyroid gland, shrinkage scar from previous neck surgery, unnamed artery in high position.

Bệnh nhân bị tụt huyết áp không nên mở khí quản qua da
Patient requires artificial ventilation with PEEP greater than 15 cm; The patient is obese, the neck is short, the landmarks are not clear; Patients under 15 years old; Displaced cervical spine fracture but not yet braced; Cervical spondylitis, unable to tilt the neck. Time of procedure: Patients in the intensive care unit need percutaneous tracheostomy when it is difficult to wean off mechanical ventilation or the patient loses the ability to protect the airways, coughs up sputum. For most patients, tracheostomy is suggested 1 to 2 weeks after intubation.
3. Perform percutaneous tracheostomy
3.1 PreparationImplementation personnel: Specialist doctors and assistants; Equipment: Percutaneous tracheostomy kit, minor surgery kit (sterile shirt, gloves, gauze, cotton swab, betadine 20ml) and Sjoberg tube, medicine,... Patient: Explained about the procedure ( purpose, procedure), increase the FiO2 of the ventilator to 100% at least 15 minutes before, relieve pain, sedation with drugs with appropriate indications, use muscle relaxants, prepare posture (head straight, maximally flexed, shoulder rested and neck cleaned). At the same time, before performing percutaneous tracheostomy, it is necessary to remove the endotracheal tube as indicated. 3.2 Implementation procedure
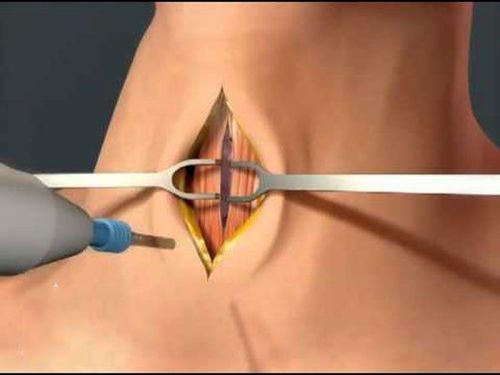
Identify landmarks, mark the position to perform percutaneous tracheostomy; Disinfect the skin of the neck area, spread a sterile towel; Locate cricoid cartilage, local anesthetic; Incision of the skin according to the marked landmarks; Tracheal cartilage cutting; Insert the Sjoberg tube, secure with sutures or surgical tape.
Ống mở khí quản
4. Complications after percutaneous tracheostomy for asphyxia
4.1 Early complications (within 24 hours after surgery)Transient hypotension; Bleeding: Occurs in most cases and may stop spontaneously; Hypoxemia: Due to hypoventilation during the procedure (the artificial ventilation system is open). To prevent this complication, before performing percutaneous tracheostomy, it is necessary to increase the volume of FiO2 by 100% to compensate and only endotracheal endoscopy should be performed to determine the correct position of the catheter; Catheter placement in the wrong position: Common in patients with short neck, thick neck fat, low tube placement, incision is not wide enough, so it is very difficult to place catheter to dilate; Perforation of the posterior tracheal wall: Catheter and dilatation can cause abrasions and perforation of the trachea, leading to subcutaneous pneumothorax, pneumothorax, and pneumomediastinum; Pneumothorax around the neck: Due to the wrong position of the catheter, injury to the trachea during dilation. This stroke can go away on its own but it can also be a sign leading to dangerous complications such as pneumomediastinum, pneumothorax; Pneumomediastinum and pneumothorax; Loss of endotracheal tube during implementation: Very dangerous, can lead to death if not detected in time; Other complications: Cardiac arrest, broken tracheal cartilage ring,...

Bệnh nhân cần được theo dõi sau phẫu thuật
Bleeding: Seen in patients with multi-organ infections, septic shock, kidney failure. This is a group of patients with coagulation disorders but not yet corrected; Granuloma formation around the base of the endotracheal tube; Tracheoesophageal fistula (rare), usually due to injury after the procedure; Tracheal stenosis, often subglottic narrowing; Percutaneous fistula persists in the cervical trachea after tracheal extubation. Percutaneous tracheostomy for asphyxia is a procedure that improves the patient's chances of survival. Like many other interventional techniques, patients may also face the risk of complications. Therefore, when performing this procedure, the patient needs to coordinate well with the doctor and follow up after the intervention closely, if there is any abnormality, it should be reported immediately for timely treatment.
Master - Doctor Cao Thanh Tam has many years of experience in the diagnosis and treatment of cardiovascular diseases; Performing transthoracic echocardiography in the field of internal medicine and interventional Cardiology; Perform other non-invasive functional investigations in the diagnosis and treatment of cardiovascular diseases. Currently working as a cardiologist at Vinmec Central Park International General Hospital since November 2015.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
SEE MORE
Things to know when intubation in children Intubation anesthesia cesarean section in patients with preeclampsia Intubation is indicated in what cases?