This is an automatically translated article.
The article is professionally consulted by Master. BSCK II Phan Thi Minh Huong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Da Nang International General Hospital.Esophageal varices are a very common symptom in patients with cirrhosis, accounting for up to 50% of patients. It is noteworthy that the mortality risk of patients with esophageal varices in the presence of cirrhosis ranges from 40 to 70%, depending on the degree of liver failure.
1. What is esophageal varices?
Esophageal varices are complications of portal hypertension, enlarged veins in the lower part of the esophagus, the tube that connects the throat and stomach. Most patients find this condition due to symptoms of gastrointestinal bleeding, vomiting blood. If not treated promptly, the patient can die.Esophageal varices occur most often in people with severe liver disease. Esophageal varices develop when normal blood flow to the liver is blocked by a blood clot or scarring in the liver. To get around the blockage, blood flows into smaller blood vessels (which are not designed for such large volumes of blood). From there, blood vessels can leak or even dilate, burst, causing bleeding and being life-threatening. Once bleeding has occurred, the risk of subsequent bleeding is significantly increased. If too much blood is lost, the patient can go into shock and at risk of death.
2. Causes of esophageal varices
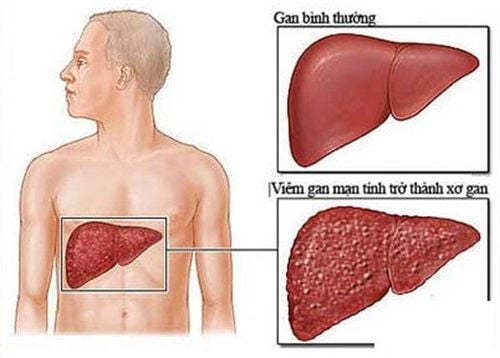
There are many causes, but esophageal varices are mainly caused by cirrhosis, occurring in nearly 30% of cirrhotic patients and accounting for nearly 80-90% of bleeding cases in these patients. Cirrhosis prevents blood flow in the portal vein - the main vein that carries blood from the stomach and intestines to the liver, increasing pressure in the portal vein and nearby veins, a phenomenon also known as hypertension. Portal vein.
Xơ gan là nguyên nhân chủ yếu gây giãn tĩnh mạch thực quản
In summary, the causes of esophageal varices include:
Severe cirrhosis, decompensated cirrhosis, some liver diseases including: hepatitis, alcoholic liver disease, fatty liver disease and cholestatic cirrhosis. A blood clot (thrombus) in the portal vein or a vein that drains into the portal vein (splenic vein) can cause esophageal varices. A parasitic infection can damage the liver, lungs, intestines, and bladder.
3. Esophageal varices in cirrhotic patients
Statistics show that up to 50% of people with cirrhosis have esophageal varices. Every year, the number of people with esophageal varices increases by about 5 - 15%. When esophageal varices turn into serious complications, esophageal veins will rupture. One third of cases of esophageal varices will rupture causing hemorrhage, which is also the main cause of death in patients with cirrhosis.If there is no cirrhosis, the mortality rate is from 5 to 10%. If accompanied by cirrhosis, the mortality rate is up to 40-70%. For patients with ruptured esophageal varices, 40% of cases stop bleeding spontaneously. However, within 6 weeks there will be 30% of bleeding again and within 1 year, the rate of rebleeding is up to 70%.
The disease will not have obvious symptoms if the patient does not have a bowel movement or vomit blood. Therefore, people with cirrhosis need to see their doctor regularly to detect the disease. If you've been diagnosed with esophageal varices, your doctor will tell you to watch out for signs of bleeding.
4. Symptoms of esophageal varices
Esophageal varices usually do not cause signs and symptoms unless bleeding is present. Signs and symptoms of bleeding from esophageal varices include:Vomiting a significant amount of blood. Black and tarry stools Shock Loss of consciousness in severe cases Accompanied by symptoms of chronic liver disease such as: jaundice, yellowing of the eyes, easy bleeding or bruising, ascites (ascites).
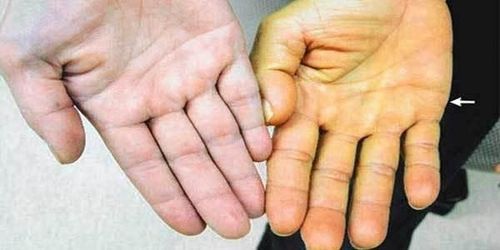
Vàng da là một trong những triệu chứng giãn tĩnh mạch thực quản
5. Prevention of esophageal varices in cirrhosis patients
For people with liver disease, in addition to using drugs as prescribed by the doctor and having regular check-ups, it is necessary to develop a scientific lifestyle regimen: do not drink alcohol, pay attention to a full diet. eating a variety of fruits and vegetables, choosing whole grains and lean protein sources, reducing the intake of fatty and fried foods, maintaining a healthy body weight, being careful when using chemicals in everyday life such as chemicals household appliances, insect sprays, etc. In particular, patients with cirrhosis need to regularly check and test blood to evaluate liver function - bile periodically. Cases of high-risk patients need to go to a medical facility for timely monitoring, diagnosis and treatment.Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.