This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
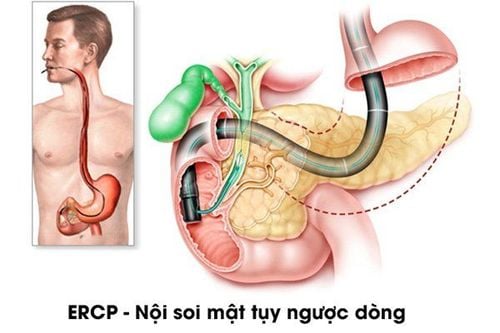
Gastrointestinal and endoscopic surgeons are familiar with the normal anatomy of the biliary tract. This article focuses on presenting the normal patterns and other changes of the biliary tract by radiographic imaging of the biliary tree to distinguish it from pathological conditions.
1. Overview
The normal diameter of the extrahepatic biliary tract is from 5.8mm, this measurement is smaller when measured by ultrasound or CT Scan because there is no injection of contrast material to cause it to dilate. When the gallbladder is removed, the bile duct is no more than 1.3cm, because the bile duct now plays a reserve role when there is no gallbladder. Therefore, if the biliary tract is larger than these numbers, there is a narrowing, chronic obstruction, or cancer.
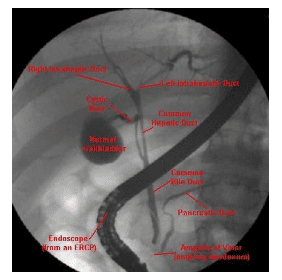
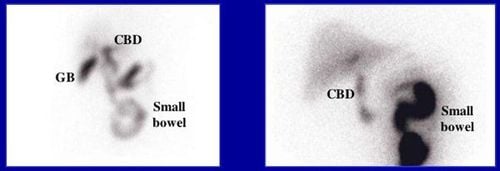
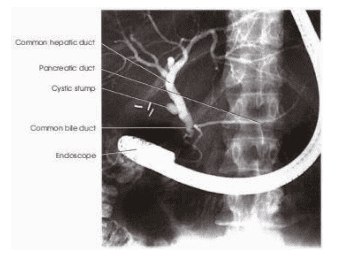
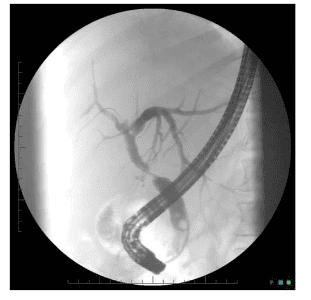
X-ray image of the biliary system when the gallbladder is intact, the diameter of the biliary tree on radiograph is not more than 1cm. Once the gallbladder is removed, when contrast is not injected into the gallbladder, the pressure in the common bile duct will be higher and the transverse diameter is now larger but not more than 1.3 cm. The intrahepatic bile duct looks like a photo of a dry tree branch. Once the image of the liver branch is not visible, it may be cirrhosis or congenital abnormalities in children, rarely in adults. In adults, when the intrahepatic biliary tract is absent, indicating some obstruction, when intrahepatic biliary visualization fails, a deep catheter is inserted to the obstruction or leads through the intrahepatic biliary branch. pump to investigate such abnormalities.
Causes of not filling the intrahepatic biliary tree: + Patient's position. The catheter rests firmly on the wall of the duct or on the gallbladder. Narrowing of the common bile duct or common hepatic duct. + Tied across the bile duct - Bile or intestinal anastomosis. + Benign liver disease: cirrhosis, stricture due to cholangitis. + Malignant liver disease: primary or secondary liver cancer. To determine, it is necessary to change the way to fill the intrahepatic biliary tract: + Change the patient's position (change of radiographic table). + Insert the catheter deeper into the biliary tract and then pump the drug. + Inflate Catheter with air balloon to block below the line. + Insert a narrow dilatation catheter or a catheter with a guide wire.
2. Normal biliary system and changes
The right hepatic bile duct system usually takes longer to absorb the drug due to the gravity of the left side lying position. Even the common bile duct is not visible, so imaging must be taken to rule out pathology more precisely. Reasons for not showing the biliary system: + Patient's position. + The cystic duct is stuck, the catheter is inserted into the distal end. + Stenosis of the common bile duct or common bile duct: benign, idiopathic, acquired, malignant. + Sew the column to the common bile duct. + Bile-enteric fistula. Methods to help take pictures of the biliary tree: + Rotate the patient's position and pump the drug. + Insert the catheter deep into the bile duct and then pump the drug. + Insert the catheter with the balloon, inflate the balloon and then pump the drug. + Or place a catheter with a selective guide to the hepatic branch and then inject drugs. Normally, with the patient lying on the left side, when contrast is injected into the biliary tract, it will easily enter the left biliary system, a small part of the right, or not until a large amount of contrast is injected or after the drug. full gallbladder. This is a false-positive sign and is not considered abnormal due to stenosis or other intrahepatic disease. It is necessary to change the patient's position, inject enough contrast material, fill the gallbladder with medicine, insert the tube into the biliary tree, use a catheter with air balloon to block the P-side system to be able to conclude the stricture.
No full biliary system: Inability to see full biliary tree may be because early filling of the gallbladder slows down the drug into the biliary tract, this usually occurs when the catheter touches the Vater papilla and does not enter the biliary tract. so the drug will enter the place of lower pressure. If the stenosis is proximal, the catheter cannot penetrate deeply into the bile duct and the drug will enter the gallbladder first. If the catheter passes through the proximal portion, the drug enters the hepatobiliary system if the biliary tract is not narrowed. If the biliary tract still cannot be imaged, a balloon catheter is inserted into the common bile duct for compression, and contrast is pumped, the biliary tract will be clearly visible even if there is stricture or liver disease such as sclerosing cholangitis.
If the catheter cannot be inserted deep into the biliary tree, then also perform contrast pump imaging with catheter blocking in the ampulla of Vater distal to the common bile duct to wait for the drug to enter the biliary system. The biliary system should be visible if there is no actual stenosis causing reflux. Inflation of the gallbladder should be avoided, causing discomfort to the patient, but if imaging of the entire biliary system is necessary, gallbladder filling should be performed with careful care. On radiographs, the right intrahepatic biliary tree looks like a tree branch, the tubular structure is evenly distributed throughout the liver.
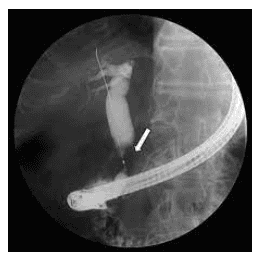
Of course, there are many other forms that mean pathology. In the absence of peripheral biliary tract, primary cirrhosis or fibrotic conditions of the biliary tract should be suspected. Another condition that causes obstruction is gallstones in the liver, which often appear in childhood. Therefore, adults with evidence of intrahepatic stones or obstructive jaundice but when cholangiography does not show the biliary tree should try to use a lead or catheter to enter the system to assess the pathology (eg. eg tumor or sclerosing cholangitis).
3. Gallbladder and changes
Usually the gallbladder is located below the liver, to the right of the common bile duct, with the exception of the gallbladder located inside the liver, higher and near the hepatic duct P. To detect gallbladder damage, there should not be too much gallbladder contrast. or too concentrated above 60%. The unusual position of the gallbladder is usually congenital. Performing endoscopic MTND in these cases is challenging, often requiring inversion of the patient's position (head rotation, P tilt). Without the pre-procedure information, it is very difficult to perform this situation.

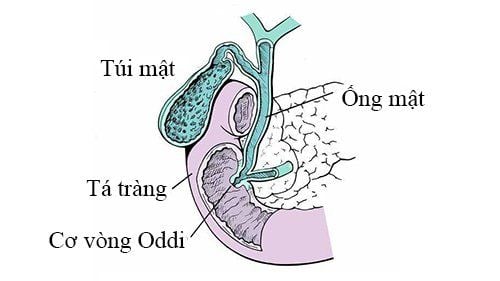
4. Abnormalities of the cystic duct
The cystic duct is an accessory branch of the main bile duct, its path varies from person to person and it can empties anywhere in the bile duct. During the contrast injection procedure, the full flow of the drug into the gallbladder can be observed. This filling defect is due to gallstones, which cannot be investigated or evaluated through SA, CT, or oral cholecystogram.
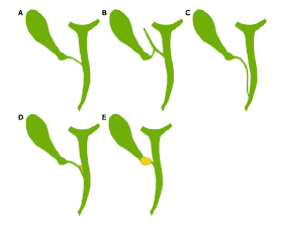
The cystic duct has many different forms when emptying into the common bile duct, the covering form means hugging the common bile duct or causing symptoms of biliary colic after eating. Turning the patient into a position allows for a comprehensive assessment of the cystic duct during autorotation. There are four different types of gallbladder, including phrygian cap and cystic gallbladder. These are rare but cannot be detected by CT or ultrasound, although these are benign. but can cause dysfunction of the expulsion contractile and thus often cause symptoms.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.