This is an automatically translated article.
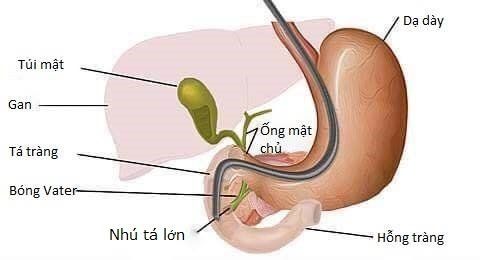
The article is professionally consulted by Master, Doctor Nguyen Ngoc Thang - Department of General Surgery, Vinmec International Hospital Da Nang.Endoscopic retrograde cholangiopancreatography is an endoscopic technique used to investigate and treat diseases of the biliary tract, pancreatic duct, and gallbladder. The bile ducts are the tubes that carry bile from the liver and gallbladder; The pancreatic duct carries pancreatic juice from the pancreas. Both of these tubes empty into the duodenum, which is the first part of the small intestine. So how is endoscopic retrograde cholangiopancreatography performed?
1. What is ERCP?
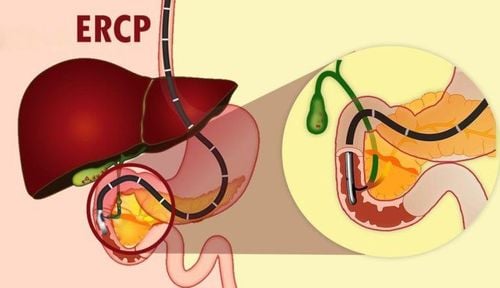
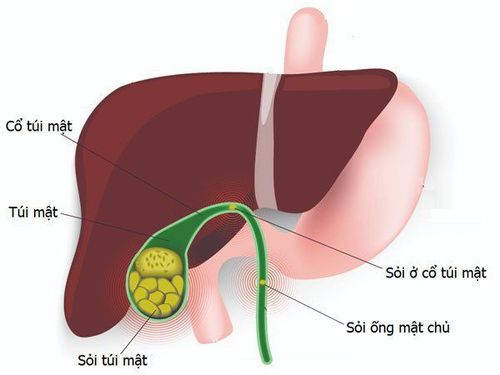
ERCP stands for "Endoscopic retrograd cholangio pancreatography", which means endoscopic retrograde cholangiopancreatography. ERCP is a procedure that can be used to diagnose and treat various diseases such as gallstones, acute pancreatitis, and chronic pancreatitis.The endoscope is an optical tube about the diameter of a little finger and can be bent easily. The endoscope is inserted through the mouth into the esophagus and down to the stomach and duodenum. The endoscope contains optical fibers that conduct light so the doctor can see inside the upper structures (gastrointestinal tract).
ERCP is performed by a gastroenterologist or surgeon who has specialized training in this technique. The scope is a long, flexible tube with a light and camera on the end. Because the procedure involves sedation or general anesthesia, the patient will be consulted by an anesthesiologist prior to the procedure.
The scope is inserted into the mouth, through the esophagus, stomach, and then to the place where the bile duct empties into the duodenum; This is called the duodenal papilla. A plastic (thin) catheter is inserted into the bronchoscope to reach the tip of the tube and then into the duodenal papilla and the bile duct. Next, the doctor will inject contrast material into the bile ducts and take X-rays. By examining the bile ducts in this way, obstructions, gallstones, tumors, or duct abnormalities can all be detected.
If abnormalities are found, the doctor may perform techniques to treat or improve the condition called ERCP surgery. For example, if a stone is found, the doctor may dilate or widen the duodenal papilla to remove the stone from the bile duct with a wire. Sphincter papillae are often cut with a cauterizer (with an electric current) during the procedure (sphincterotomy), allowing for better drainage of the bile ducts. If there is a narrowing of the bile duct, the doctor will place a short plastic or metal tube called a stent into the narrowing to drain the bile.
2. What preparation is required for ERCP?

Không nên ăn vài giờ trước thủ thuật
Do not eat for several hours before the procedure. You are allowed to drink some water up to 2 hours before the test. Medications that need to be stopped before the procedure. Antibiotics may be needed depending on the purpose.
3. How is ERCP performed?
Your doctor may first numb the back of your throat with a topical anesthetic spray. You are usually given a sedative into a vein in your arm. Sedatives make you drowsy and relaxed but do not induce sleep. This is not general anesthesia.The patient is lying on his side on the bed and the doctor will ask him to swallow the end of the endoscope. Modern endoscopes are usually smaller than the index finger and quite easy to swallow. The doctor gently pushes the scope down the esophagus, stomach, and into the duodenum.
The doctor will look at the inside of your stomach and duodenum through a monitor connected to the endoscope. Air is then pumped into the stomach and duodenum through a channel in the endoscope, which helps to stretch the surface and make it easier to see. You may feel bloated and want to burp.
The endoscope also has a side channel for instruments to pass through, which is used by the doctor for a variety of purposes. Example:
Injecting contrast material into the bile duct or pancreatic duct. X-ray films will be taken shortly afterwards to record the details in the tube. Contrast injection may also show ductal stenosis, stone entrapped in duct, or ductal tumor compression... Biopsy of the medial duodenum, stomach, bile duct, and pancreatic duct proximal to the papilla. The biopsy sample will be viewed under a microscope to look for abnormal tissues and cells. If the X-ray shows a gallstone stuck in the duct, the doctor will widen the papilla to allow the stone to drain into the duodenum. If radiographs show narrowing or blockage of the bile duct, the doctor may place a stent to widen the lumen. This stent allows bile to flow down the duodenum in a natural way and can stay permanently in place without the patient feeling it.
Nội soi mật tụy ngược dòng
4. What happens after ERCP?
ERCP is done for X-rays only, most people can go home after resting for a few hours. You should not drive, operate machinery, or drink alcohol for 24 hours after taking the sedative. If you go home on the day of the procedure, you will need someone to accompany you and stay with you for 24 hours until the sedation wears off completely. Most people can return to normal activities after 24 hours.5. Does ERCP have any side effects or complications?
Most ERCPs are performed safely and without problems. Some people have a mild sore throat a few days later. You may feel tired or drowsy for a few hours due to the sedation. Uncommon complications include: damage to the intestine, bile duct or pancreatic duct by the endoscope, which can cause bleeding, infection and, rarely, perforation.If any of the following symptoms occur within 48 hours of ERCP, see your doctor for re-examination:
Abdominal pain - especially pain that is progressive, severe, and of a nature different from heartburn, difficulty normal consumption. Fever. Shortness of breath. Vomiting/vomiting blood. Pancreatitis: This complication can be serious in some cases.