This is an automatically translated article.
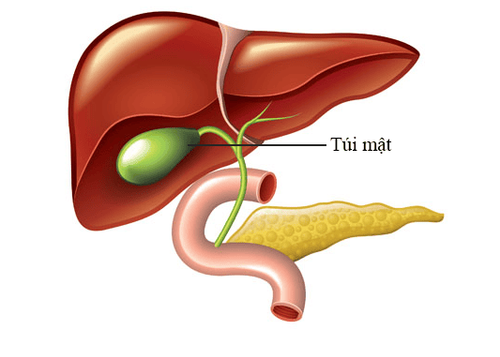
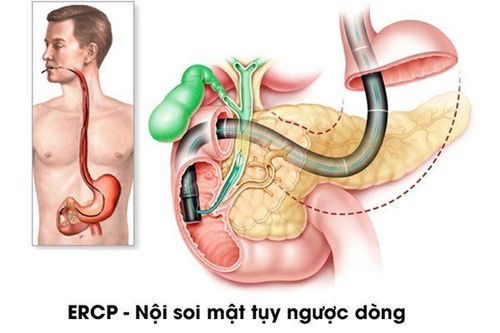
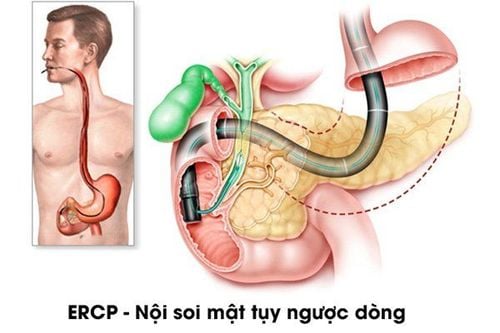
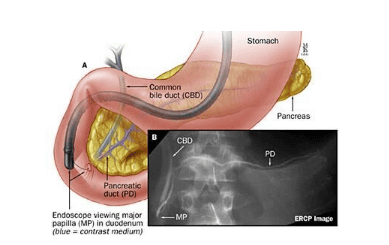
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalBeginning in 1968, endoscopic retrograde cholangiopancreatography (ERCP) was a turning point in the diagnosis and treatment of pancreatic diseases. Therefore, an accurate indication for this screening is important given the potential side effects associated with the procedure. Early recognition and appropriate management of potential adverse events are essential to reduce associated morbidity and mortality.
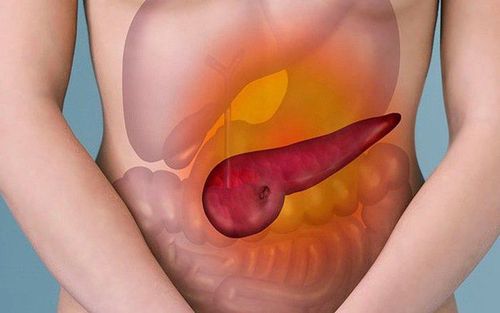
As in other endoscopic procedures, there are determinants of safety for ERCP, in addition to the exact indication, clinical status of the patient, age, sex, type of sedation used, type of procedure The surgical technique performed, the use of appropriate accessories, and the training of the endoscopist and assistant are considered. Acute pancreatitis is the most common serious complication following ERCP, often confused with elevations in serum amylase levels that occur in 75% of patients. Clinically acute pancreatitis itself, defined as a clinical syndrome of abdominal pain and hyperplasia requiring hospitalization, is much less common than its presentation. There is still some controversy in the literature on this topic. The purpose of this review is to provide up-to-date information on acute pancreatitis after ERCP and its prevention.
Kỹ thuật nội soi mật tụy ngược dòng
1. Physiology
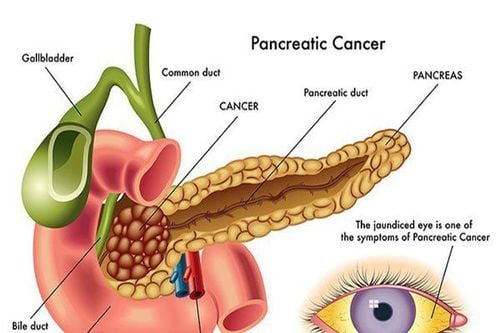
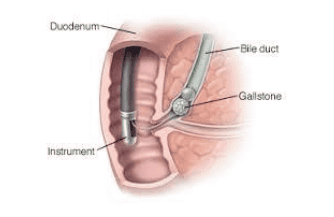
The determinants of the inflammatory process in the pancreas are multifactorial. Several factors have been suggested that may act alone or in combination to induce post-ERCP pancreatitis (acute post-endoscopic retrograde cholangitis). The two most important injuries are the mechanical damage caused by the instrument in the pancreatic duct and the hydrostatic injury caused by the injection of contrast. During ERCP and sphincterotomy, the pancreas is exposed to various forms of trauma: mechanical, chemical, hydrostatic, thermal, and even allergic. It is well known that prolonged manipulation around the papillary foramen, accidental opening into the pancreatic duct, and repeated injections into the pancreatic duct are common when selective dilation of the bile duct is difficult. This can lead to mechanical damage to the duct or papilla. Thermal injury to the electrocautery current can also produce edema of the pancreatic duct orifice, leading to ductal obstruction, affecting pancreatic secretions Hydrostatic injury due to excessive injection of contrast agent. Pancreatic duct irradiation is probably an important cause of acute pancreatitis after endoscopic retrograde cholangiopancreatitis. Be it an allergy or a chemical injury, the contrast medium can lead to injury. In a study by George et al., there were no statistically significant differences between contrast categories in the analysis of randomized studies.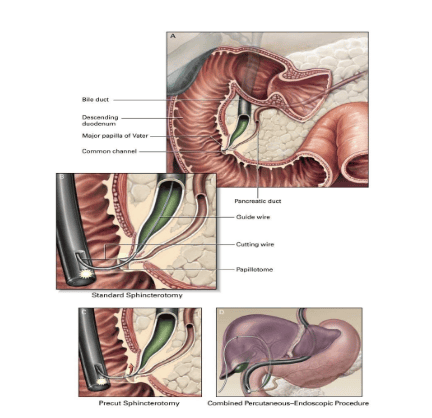
Các kỹ thuật cắt cơ vòng Oddi trong nội soi mật tụy ngược dòng
2. Epidemiology and risk factors
Incidence
The incidence of pancreatitis after ERCP can vary from 1% to 10%, reaching alarming levels of 30% in high-risk patients. Stratification of the severity of acute pancreatitis after examination revealed a prevalence of 3.6% to 4% for mild acute pancreatitis, 1.8% to 2.8% for moderate acute pancreatitis, and 0. 3% to 0.5% for severe acute pancreatitis with a mortality rate of 0.2%. Higher rates were observed in patients evaluated for possible sphincter of Oddi dysfunction
Risk factors
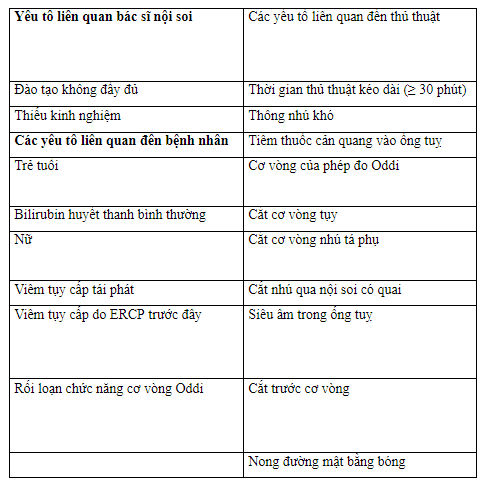
According to European Society of Gastroenteroscopy (ESGE) guidelines [ 20 ] and American Society of Gastroenteroscopy (ASGE): History of pancreatitis, suspected sphincter of Oddi dysfunction, female gender, and young age are certainly “patient-related risk factors” for with acute pancreatitis after endoscopic retrograde cholangiopancreatitis. On the other hand, difficult papillary catheterization, pancreatic injection, and use of anterior resection are “procedural-related risk factors.
Patient-related factors
There are several patient-related factors, the most common factors being female sex, normal bilirubin levels, young age, history of recurrent acute pancreatitis, and disease patients with suspected sphincter of Oddi dysfunction. Patients with a history of chronic pancreatitis have a protective effect against acute pancreatitis after endoscopic retrograde cholangiopancreatitis. Unfortunately, the risk factors add up. For example, the combination of female sex, patients with suspected sphincter of Oddi dysfunction, young age, difficult papillary communication, bilirubin within the normal range, and the absence of common bile duct stones have a greater than 40 percent risk of developing pancreatitis. %. Factors related to the endoscopist
These are the most subjective. The experience of the endoscopist, the presence of interns, and multiple operators are believed to be an independent risk factor for acute pancreatitis after endoscopic retrograde cholangiopancreatitis.
Procedural-related factors
Procedure-related factors are best studied and discussed in the literature. Anterior resection technique, commonly used in difficult ERCP cases, the time and number of papillary catheterizations, trauma, and edema of the duodenal papilla (large papilla) due to the number of attempts are independent factors for the Acute pancreatitis after endoscopic retrograde cholangiopancreatitis. In a systematic review with meta-analysis including 25 randomized controlled trials (RCTs) evaluating the incidence of acute pancreatitis after endoscopic retrograde cholangiopancreatectomy in patients undergoing sphincterotomy, Large duodenal papillary biliaryectomy without sphincterotomy and with patients undergoing both procedures, it was concluded that the incidence of acute pancreatitis after endoscopic retrograde cholangiopancreatitis was similar between groups.
Thời gian thông nhú kéo dài là yếu tố nguy cơ của viêm tụy sau ERCP
3. Risk factors for acute pancreatitis after endoscopic retrograde cholangiopancreatitis in relation to the operator and procedure.
4. Clinical manifestations
The clinical manifestations of acute pancreatitis after endoscopic retrograde cholangiopancreatitis are similar to those seen in patients with acute pancreatitis of other etiologies. These include right epigastric or upper quadrant pain, abdominal pain, and elevated amylase and lipase levels. Acute pancreatitis after ERCP can be classified as mild, moderate, or severe based on the American Gastroenterology Association and the American College of Gastroenterology: (1) mild amylase levels 24 h after examination, maintained above up to three times the reference value at admission; (2) average need for hospitalization from 4 to 10 days; and (3) severe severity requiring hospitalization for more than 10 days or requiring invasive treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.